Insulin-pump therapy pada anak dengan diabetes melitus tipe 1: Studi literatur
Abstract
Background: Diabetes Mellitus (DM) is a metabolic disease characterized by an increase in blood glucose levels above normal values. This is caused by impaired glucose metabolism due to insulin deficiency, both relative and absolute. Diabetes that is often found in children is Diabetes Mellitus Type 1 (T1DM), this case is a disease that cannot be cured and requires lifelong treatment. It is estimated that every year 128,900 children and adolescents are diagnosed with Type 1 Diabetes Mellitus (T1DM). Globally in 2019 around 1,110,000 children and adolescents were diagnosed with T1DM. Nearly 80% of diabetes deaths occur in low- and middle-income countries. According to the World Health Organization (WHO), India is the country with the largest number in the world with more than 32 million diabetes mellitus patients and this number is predicted to increase to 79.4 million by 2030.
Purpose: To reduce the risk of long-term complications, maintain HbA1C on target, and provide knowledge, education and skills to care for children with T1DM until adulthood independently.
Method: This research uses a literature review design, namely collecting and summarizing various results from previous research to analyze literature that has been selected from various sources to form a conclusion on new ideas or ideas. The literature study selection process was adapted from Preferred Reporting Items for Systematic Reviews (PRISMA-ScR). The journals used in this study are journals that discuss topics with three keyword categories, namely, Insulin Pump, Diabetes Mellitus Type, and Pediatrics. Search for articles via online databases, including Scopus, ProQuest, Clinical Key Nursing, Sage, and Google Scholar, published in the last five years between 2019-2023.
Results: The results of the study are based on a literature review that the author found that the use of insulin pumps is very effective in children and adolescents. In several developed countries, the use of insulin pumps is funded by the local government, but in several rural areas the use of this technology still faces many obstacles and Also, the price of an insulin pump is not cheap, which is an inhibiting factor for blood sugar instability for T1DM.
Conclusion: Children with T1DM need insulin throughout their lives, the use of an insulin pump is very effective in controlling blood sugar. The use of an insulin pump can reduce punctures for daily blood sugar monitoring checks and is able to read the condition of glycemic levels in the blood equipped with a sensor. However, the high price of insulin pumps makes families think twice about buying insulin pumps. Insulin pumps can only be purchased by those with above average economic conditions. In developed countries such as Canada, the use of insulin pumps is funded by the local government. However, in developing countries, low ability and purchasing power combined with difficult access to technology mean that not all T1DM sufferers receive adequate treatment. In Indonesia, not many pediatric patients use insulin pumps, only patients from well-off families can use this technology. Apart from that, this insulin pump is not covered by insurance, either government insurance such as National Health Insurance (JKN) or private insurance. So this problem needs to be of concern to various elements, both health and government.
Keywords: Child; Diabetes Mellitus Type 1 (T1DM); Insulin Pump; Therapy.
Pendahuluan: Diabetes Mellitus (DM) merupakan penyakit metabolik yang ditandai dengan peningkatan kadar glukosa darah diatas nilai normal. Hal ini disebabkan oleh adanya gangguan metabolisme glukosa akibat kekurangan insulin baik secara relatif maupun absolut. Diabetes yang sering ditemui pada anak-anak adalah Diabetes Mellitus Tipe 1 (DMT1), kasus ini merupakan penyakit yang belum dapat disembuhkan dan memerlukan perawatan seumur hidup. Diperkirakan setiap tahun terdapat 128.900 anak-anak dan remaja di diagnosis Diabetes Melitus Tipe 1 (DMT1). Secara global pada tahun 2019 sekitar 1.110.000 anak-anak dan remaja didiagnosis DMT1. Hampir 80% kematian diabetes terjadi di negara berpenghasilan rendah dan menengah. Menurut World Health Organization (WHO), India adalah negara yang mempunyai jumlah terbesar di dunia dengan lebih dari 32 juta pasien diabetes mellitus dan jumlah ini diprediksikan meningkat menjadi 79.4 juta pada tahun 2030.
Tujuan: Untuk menurunkan risiko komplikasi jangka panjang, mempertahankan HbA1C sesuai target, dan memberikan pengetahuan, pendidikan, serta keterampilan untuk merawat anak penderita DMT1 hingga dewasa secara mandiri.
Metode: Penelitian ini menggunakan rancangan literature review yaitu melakukan pengumpulan dan merangkum berbagai hasil dari penelitian sebelumnya untuk menganalisis literatur- literatur yang telah dipilih dari berbagai sumber hingga menjadi sebuah satu kesimpulan ide atau gagasan baru. Proses pemilihan studi literatur diadaptasi dari Preferred Reporting Items for Systematic Reviews (PRISMA-ScR). Jurnal yang digunakan dalam studi ini adalah jurnal-jurnal yang membahas topik dengan tiga kategori kata kunci yakni, Insulin Pump, Diabetes Mellitus Type, dan child. Penelusuran artikel melalui online database antara lain, Scopus, ProQuest, Clinical Key Nursing, Sage, dan Google Scholar yang diterbitkan lima tahun terakhir antara 2019-2023.
Hasil: Hasil telaah berdasarkan literatur review yang penulis dapatkan Bahwa penggunaan insulin pump sangat efektif digunakan pada anak-anak dan remaja, di beberapa negara maju penggunaan insulin pump di biayai oleh pemerintah setempat, tetapi di beberapa daerah pedesaan penggunaan teknologi ini masih banyak mengalami kendala dan juga harga insulin pump yang tidak murah menjadi faktor penghambat ketidakstabilan gula darah untuk DMT1.
Simpulan: Anak-anak dengan DMT1 membutuhkan insulin sepanjang hidup mereka, penggunaan insulin pump sangat efektif di dalam mengontrol gula darah. Penggunaan insulin pump mampu mengurangi tusukan untuk pemeriksaan monitoring gula darah harian dan mampu membaca kondisi kadar glikemik dalam darah dilengkapi dengan sensor. Tetapi harga insulin pump yang mahal membuat keluarga berpikir ulang membeli alat insulin pump, insulin pump hanya mampu dibeli oleh mereka yang mempunyai ekonomi diatas rata-rata. Di negara maju seperti Kanada penggunaan insulin pump didanai oleh pemerintah setempat. Namun di negara berkembang, kemampuan dan daya beli yang rendah ditambah sulitnya akses teknologi sehingga tidak semua penderita DMT1 mendapatkan perawatan yang memadai. Di Indonesia sendiri belum banyak pasien anak yang menggunakan insulin pump, hanya pasien yang berasal dari keluarga mampu yang dapat menggunakan teknologi tersebut. Selain itu, insulin pump ini tidak ditanggung oleh asuransi baik asuransi pemerintah seperti Jaminan Kesehatan Nasional (JKN) maupun asuransi swasta. Sehingga permasalahan ini perlu menjadi perhatian dari berbagai elemen baik kesehatan maupun pemerintahan.
Keywords
References
Abujaradeh, H., Viswanathan, P., Galla, B. M., Sereika, S. M., DiNardo, M., Feeley, C. A., & Charron-Prochownik, D. (2021). Trait mindfulness and mindfulness practices in adolescents with type 1 diabetes: descriptive and comparative study. Journal of Pediatric Health Care, 35(6), 592-600.
Adelita, M., Arto, K. S., & Deliana, M. (2020). Kontrol Metabolik pada Diabetes Melitus Tipe-1. Cermin Dunia Kedokteran, 47(3), 227-232.
Al Hayek, A. A., Robert, A. A., & Al Dawish, M. A. (2021). Effectiveness of the freestyle libre 2 flash glucose monitoring system on diabetes-self-management practices and glycemic parameters among patients with type 1 diabetes using insulin pump. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 15(5), 102265.
Alvarenga, C. S., La Banca, R. O., Neris, R. R., de Cassia Sparapani, V., Fuentealba-Torres, M., Cartagena-Ramos, D., & Nascimento, L. C. (2022). Use of continuous subcutaneous insulin infusion in children and adolescents with type 1 diabetes mellitus: a systematic mapping review. BMC endocrine disorders, 22(1), 1-15.
Christian, B. J. (2020). Translational Research-Promoting Quality of Life and Reducing Health Disparities Among Children with Chronic Conditions and their Families. Journal of pediatric nursing, 55, 258-260.
Haddadi, D., Rosolowsky, E., Pacaud, D., McKeen, J., Young, K., Madrick, B., & Clinical Advisory Committee. (2021). Revision of Alberta’s Provincial Insulin Pump Therapy Criteria for Adults and Children With Type 1 Diabetes: Process, Rationale and Framework for Evaluation. Canadian Journal of Diabetes, 45(3), 228-235.
Harsismanto, J., Padila, P., Andri, J., Sartika, A., & Andrianto, M. B. (2021). Kualitas Hidup Pasien Diabetes Melitus Tipe 2. Jurnal Kesmas Asclepius, 3(2), 80-87.
Hedge, V., Carter, K., Downey, W., & Sharp, H. (2023). Prevalence of Diabetes Distress Among Adolescents With Type 1 Diabetes Mellitus. The Journal for Nurse Practitioners, 19(3), 104383.
Holt, R. I., DeVries, J. H., Hess-Fischl, A., Hirsch, I. B., Kirkman, M. S., Klupa, T., & Peters, A. L. (2021). The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes care, 44(11), 2589-2625.
Hughes, M. S., Bailey, R., Calhoun, P., Shah, V. N., Lyons, S. K., & DeSalvo, D. J. (2022). Off‐label use of sodium glucose co‐transporter inhibitors among adults in type 1 diabetes exchange registry. Diabetes, Obesity and Metabolism, 24(1), 171-173.
Hwang, N. (2022). Advanced technology used in pediatric type 1 diabetes management. Journal of Pediatric Nursing, S0882-5963.
Jewell, V. D., Wise, A. C., Knezevich, E. L., Abbott, A. A., Feiten, B., & Dostal, K. (2023). Type 1 Diabetes Management and Health Care Experiences Across Rural Nebraska. Journal of Pediatric Health Care, 37(1), 48-55.
O'Connor, M. R., Carlin, K., Coker, T., Zierler, B., & Pihoker, C. (2019). Disparities in insulin pump therapy persist in youth with type 1 diabetes despite rising overall pump use rates. Journal of Pediatric Nursing, 44, 16-21.
Özgen Saydam, B. A. Ş. A. K., Adiyaman, S., Yeşilli, B., Bektas, A., Vatansever, O., Aydin, N., & Akinci, B. (2022). Simultaneous Teamwork May Improve Hypoglycemia Rates in Patients with Type 1 Diabetes Using an Insulin Pump. Turkish Journal of Endocrinology and Metabolism, 26(1).
Perkins, B. A., Sherr, J. L., & Mathieu, C. (2021). Type 1 diabetes glycemic management: Insulin therapy, glucose monitoring, and automation. Science, 373(6554), 522-527.
Saydam, B. O., Adiyaman, S. C., Demir, T., Comlekci, A., & Yener, S. (2022). The use of low dose prednisolone in patients with subacute thyroiditis and its effect on impaired life and sleep quality. Acta Endocrinologica (Bucharest), 18(1), 64.
Setyawati, A. D., Padila, P., & Andri, J. (2020). Obesity and Heredity for Diabetes Mellitus among Elderly. JOSING: Journal of Nursing and Health, 1(1), 26-31.
Sinaga, M. R. B., Yensuari, Y., & Dharma, S. (2023). Pengaruh Kendali Glukosa Darah, Hipertensi, Dan Dislipidemia Terhadap Komplikasi Retinopati Diabetik Pada Penderita Diabetes Melitus Tipe 2. Jurnal Multidisiplin Indonesia, 2(10), 3304-3319.
Song, C., Booth, G. L., Perkins, B. A., & Weisman, A. (2021). Impact of government-funded insulin pump programs on insulin pump use in Canada: a cross-sectional study using the National Diabetes Repository. BMJ Open Diabetes Research and Care, 9(1), e002371.
Woerner, S. (2014). The benefits of insulin pump therapy in children and adolescents with type 1 diabetes. Journal of pediatric nursing, 29(6), 712-713.
Zhang, L., Xu, H., Liu, L., Bi, Y., Li, X., Kan, Y., & Zhang, Y. (2022). Related factors associated with fear of hypoglycemia in parents of children and adolescents with type 1 diabetes-A systematic review. Journal of pediatric nursing, 66, 125-135.
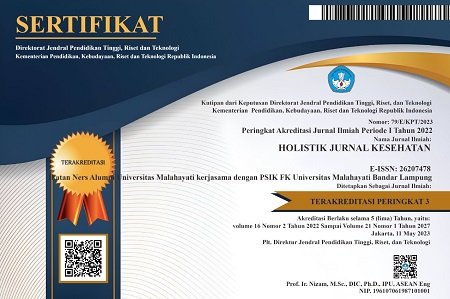
DOI: https://doi.org/10.33024/hjk.v17i7.12869
Refbacks
- There are currently no refbacks.
Copyright (c) 2023 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.