Intervensi selama kehamilan untuk mencegah kelahiran prematur: Systematic literature review
Abstract
Interventions during pregnancy to prevent preterm birth: A systematic literature review
Background: Premature birth is a major factor that contributes to mortality of newborns globally and impacts long-term to health problems for survivors. Premature births have increased in the last 20 years where the phenomenon is equivalent to 1 in 10 births each year. Therefore, prevention of preterm labor is important given to pregnant women.
Purpose: This study aimed to find out effectiveness interventions during pregnancy to preventing preterm birth.
Method: The design used literature review, articles were collected using search engines such as Academic Search Complete (EBSCO) as many as 78 articles, CINAHL (EBSCO) 36 articles, Science Direct 593 articles, and PUBMED 55 articles. From the predetermined article criteria, it found 3 articles from 762 that correspond to different interventions, namely consumption of progesterone supplements, cognitive behavior to reduce cigarette smoke exposure, and early detection in pregnant women at high risk of preterm delivery.
Results: The result showed that there were 3 interventions in the effort to prevent preterm birth, namely: progesterone supplementation therapy, the intervention to reduce exposure to cigarette smoke in the environment, and identification and management of early detection of fast on pregnant women at high risk of preterm birth.
Conclusion and Recommendation: several interventions can use in preventing preterm birth of pregnant women effectively, such as progesterone supplementation, reduction in cigarette smoke exposure in pregnant women, and early detection of pregnancy. Further research is suggested by involving the role of the family in preventing premature birth
Keywords: Intervention; Pregnant women; Premature birth; Prevention
Pendahuluan: Kelahiran prematur merupakan faktor mayor yang berkontribusi terhadap kematian bayi baru lahir secara global dan berdampak pada masalah kesehatan jangka panjang untuk bayi yang selamat. Kelahiran prematur mengalami peningkatan pada 20 tahun terakhir dimana fenomenanya setara dengan 1 dari 10 kelahiran tiap tahunnya. Oleh karena itu pencegahan persalinan prematur penting diberikan kepada ibu hamil.
Tujuan: untuk mengetahui intervensi efektif selama kehamilan dalam mencegah persalinan prematur.
Metode: Desain yang digunakan adalah literature review, artikel dikumpulkan menggunakan mesin pencarian seperti Academic Search Complete (EBSCO) 78 articles, CINAHL (EBSCO) 36 articles, Science Direct 593 articles, dan PUBMED 55 articles. Dari kriteria inklusi artikel yang telah ditentukan, ditemukan 3 artikel dari 762 yang sesuai dengan intervensi yang berbeda.
Hasil: menunjukan bahwa ada 3 intervensi dalam upaya mencegah kelahiran prematur yaitu: terapi suplementasi progesteron, intervesi pengurangan paparan asap rokok pada lingkungan, dan identifikasi dan penatalaksanaan deteksi dini secara cepat terhadap ibu hamil yang berisiko tinggi lahir prematur.
Simpulan dan Saran: Intervensi pemberian suplemen progesteron, pengurangan paparan asap rokok di lingkungan ibu hamil, dan deteksi dini pada kehamilan terbukti efektif dalam mencegah kelahiran prematur pada ibu hamil. Disarankan penelitian lebih lanjut dengan melibatkan peran keluarga dalam mencegah kelahiran prematur.
Keywords
Full Text:
PDFReferences
Anderson, L., Martin, W., Higgins, C., Nelson, S. M., & Norman, J. E. (2009). The effect of progesterone on myometrial contractility, potassium channels, and tocolytic efficacy. Reproductive sciences, 16(11), 1052-1061.
El-Mohandes, A. A., Kiely, M., Blake, S. M., Gantz, M. G., & El-Khorazaty, M. N. (2010). An intervention to reduce environmental tobacco smoke exposure improves pregnancy outcomes. Pediatrics, 125(4), 721-728.
Fayed, N. M. (2016). Effect of Physical Stimulation on Premature Very Low Birth Weight Infants. American Journal of Nursing Research, 4(1), 6-12.
Hutchins, S. S., Brown, C., Mayberry, R., & Sollecito, W. (2015). Value of a small control group for estimating intervention effectiveness: results from simulations of immunization effectiveness studies. Journal of comparative effectiveness research, 4(3), 227-238.
Ibrahim, M., Ramy, A. R. M., & Younis, M. A.-F. (2010). Progesterone supplementation for prevention of preterm labor: a randomized controlled trial. Middle East Fertility Society Journal, 15(1), 39-41.
Institute, J. B. (2017). The Joanna Briggs Institute Critical Appraisal tools for use in JBI systematic reviews. Checklist for Randomized Controlled Trials.
Lassi, Z. S., Middleton, P. F., Crowther, C., & Bhutta, Z. A. (2015). Interventions to improve neonatal health and later survival: an overview of systematic reviews. EBioMedicine, 2(8), 985-1000.
Maggio, L., & Rouse, D. J. (2014). Progesterone. Clinical obstetrics and gynecology, 57(3), 547-556.
Medley, N., Vogel, J. P., Care, A., & Alfirevic, Z. (2018). Interventions during pregnancy to prevent preterm birth: an overview of Cochrane systematic reviews. Cochrane Database of Systematic Reviews(11).
Meis, P. J., Klebanoff, M., Thom, E., Dombrowski, M. P., Sibai, B., Moawad, A. H., & Varner, M. W. (2003). Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. New England Journal of Medicine, 348(24), 2379-2385.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine, 151(4), 264-269.
Newnham, J. P., Kemp, M. W., White, S. W., Arrese, C. A., Hart, R. J., & Keelan, J. A. (2017). Applying precision public health to prevent preterm birth. Frontiers in public health, 5, 66.
Noriani, N. K., Putra, I. A. E., & Karmaya, M. (2015). Paparan asap rokok dalam rumah terhadap risiko peningkatan kelahiran bayi prematur di Kota Denpasar. Public Health and Preventive Medicine Archive, 3(1), 68-73.
Norton, M. E., Chauhan, S. P., Dashe, J. S., & Medicine, S. f. M.-F. (2015). Society for maternal-fetal medicine (SMFM) clinical guideline# 7: nonimmune hydrops fetalis. American journal of obstetrics and gynecology, 212(2), 127-139.
O'brien, J., Defranco, E., Adair, C., Lewis, D., Hall, D., How, H., & Creasy, G. (2009). Effect of progesterone on cervical shortening in women at risk for preterm birth: secondary analysis from a multinational, randomized, double‐blind, placebo‐controlled trial. Ultrasound in Obstetrics and Gynecology, 34(6), 653-659.
Patel, A., Prakash, A. A., Pusdekar, Y. V., Kulkarni, H., & Hibberd, P. (2017). Detection and risk stratification of women at high risk of preterm birth in rural communities near Nagpur, India. BMC pregnancy and childbirth, 17(1), 311.
Roelands, J., Jamison, M. G., Lyerly, A. D., & James, A. H. (2009). Consequences of smoking during pregnancy on maternal health. Journal of Women's Health, 18(6), 867-872.
WHO. (2018). Preterm birth Retrieved April 7, 2020, 2020, from https://www.who.int/news-room/fact-sheets/detail/preterm-birth
Zhang, Y.-P., Liu, X.-H., Gao, S.-H., Wang, J.-M., Gu, Y.-S., Zhang, J.-Y., & Li, Q.-X. (2012). Risk factors for preterm birth in five Maternal and Child Health hospitals in Beijing. PLoS One, 7(12).
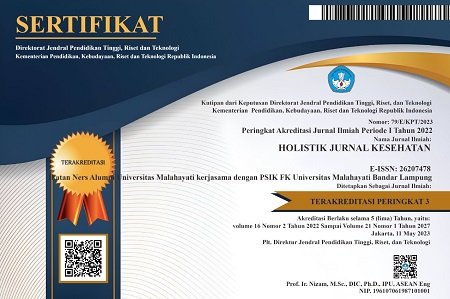
DOI: https://doi.org/10.33024/hjk.v14i2.2685
Refbacks
Copyright (c) 2020 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.