Pengaruh Buerger Allen Exercise terhadap sirkulasi ekstremitas bawah bagi penyandang diabetes melitus
Abstract
Background: Buerger Allen Exercise is a specific exercise intended to improve circulation to the feet and leg using gravitational changes to influence the distribution of body fluids to alternately help emptying and fulfilling the blood columns, and by using muscle contraction through active movement of the ankle to improve circulation of peripheral blood vessel by driving blood and blood vessel. Ankle Brachial Index (ABI) is one of the indicators to assess changes in peripheral vascularization.
Purpose: To know the effectiveness of Buerger Allen Exercise on lower limb circulation among patients with diabetes mellitusMethod: A quasi-experimental by pre- and post-test with controlled group, involving 28 participants divided by two group; interventional group and controlled group. The sampling technique is a non-probability sampling.
Results: Shows by t-test and GLM-RM finds out that there are significant differences in the improvements of ABI average scores between interventional and controlled groups after Buerger Allen Exercise is conducted to the right leg with (p-value= 0.001; α = 0.05 ) and to the left leg with (p-value= 0.002; α = 0.05). While, GLM-RM in the research is still not able to determine the optimal point of time in practicing Buerger Allen Exercise.
Conclusion: The effectiveness of Buerger Allen Exercise on lower limb circulation and suggestion that Buerger Allen Exercise can be applied as one of the nurse self-intervention to improve peripheral vascularization to patients with diabetes mellitus
Keywords : Buerger Allen Exercise; Lower limb circulation; patients; diabetes mellitus
Pendahuluan: Buerger Allen Exercise adalah latihan khusus yang ditujukan untuk meningkatkan sirkulasi ke kaki dengan menggunakan perubahan gravitasi mempengaruhi distribusi cairan dalam tubuh dengan membantu secara bergantian untuk mengosongkan dan mengisi kolom darah, dan menggunakan kontraksi otot melalui gerakan aktif dari pergelangan kaki untuk meningkatkan sirkulasi pembuluh darah perifer dengan menggerakan darah dan pembuluh darah. Ankle Brachial Index (ABI) merupakan salah satu indikator untuk menilai perubahan vaskularisasi perifer.
Tujuan: Untuk mengetahui pengaruh Buerger Allen Exercise terhadap sirkulasi ekstremitas bawah bagi penyandang diabetes melitus
Metode : Menggunakan desain kuasi eksperimen pre post tes dengan kelompok kontrol, melibatkan 28 partisipan yang dibagi dalam dua kelompok; kelompok intervensi dan kelompok kontrol. Tehnik pengambilan sampel dengan non probability sampling. Penelitian ini menggunakan t-tes dan GLM-RM.
Hasil : Uji t-tes didapatkan perbedaan yang signifikan rata-rata skor peningkatan ABI antara kelompok intervensi dan kontrol setelah dilakukan Buerger Allen Exercise pada kaki kanan dengan (p-value= 0,001; α = 0,05 ) dan pada kaki kiri dengan (p-value= 0,002; α = 0,05 ). Sedangkan dengan GLM-RM pada penelitian ini belum dapat menentukan titik optimum waktu pelaksanaan Buerger Allen Exercise.
Simpulan: Adanya pengaruh Buerger Allen Exercise terhadap sirkulasi ekstremitas bawah dan disarankan agar Buerger Allen Exercise dapat diterapkan sebagai salah satu intervensi mandiri perawat dalam meningkatkan vaskularisasi perifer bagi penyandang diabetes melitus
Keywords
Full Text:
PDFReferences
Abhilash, M., & Augustine, R. (2014). Diabetes and Health Care: An Overview. Diabetes Mellitus and Human Health Care: A Holistic Approach to Diagnosis and Treatment, 1.
Al-Daghri, N. M., Al-Attas, O. S., Alokail, M. S., Alkharfy, K. M., Yousef, M., Sabico, S. L., & Chrousos, G. P. (2011). Diabetes mellitus type 2 and other chronic non-communicable diseases in the central region, Saudi Arabia (Riyadh cohort 2): a decade of an epidemic. BMC medicine, 9(1), 76.
Allen, A. W. (1931). The general management of circulatory disorders of the extremities. New England Journal of Medicine, 204(17), 859-862.
Ballaz, L., Fusco, N., Crétual, A., Langella, B., & Brissot, R. (2007). Acute peripheral blood flow response induced by passive leg cycle exercise in people with spinal cord injury. Archives of physical medicine and rehabilitation, 88(4), 471-476.
Black, J. M., & Hawks, J. H. (2014). Text book of medical surgical nursing. Philadelphia: WB Saunders company publication, 473-500.
Bottomley, J. M. (2007). The insensitive foot. Geriatric Rehabilitation Manual, 2nd Edition, Churchill Livingstone, Edinburgh, 333-343.
Brayant, R. A., & Nix, D. P. (2015). Acute & chronic wounds. Current Management Concepts. Third Edition. United States of America: Mosby Elsevier.
Buerger, L. (1924). The Circulatory Disturbances of the Extremities: Including Gangrene, Vasomotor, and Trophic Disorders. WB Saunders Company.
Eliana, F., SpPD, K. E. M. D., & Yarsi, B. P. D. F. (2015). Penatalaksanaan DM Sesuai Konsensus Perkeni 2015. PB. Perkeni. Jakarta.
Fatimah, R. N. (2015). Diabetes melitus tipe 2. Jurnal Majority, 4(5).
Fitri, E., Andayani, T. M., & Suparniati, E. (2015). Cost analysis of diabetes mellitus. Jurnal Manajemen Dan Pelayanan Farmasi (Journal of Management and Pharmacy Practice), 5(1), 61-66.
Fowkes, F. G. R., Rudan, D., Rudan, I., Aboyans, V., Denenberg, J. O., McDermott, M. M., & Criqui, M. H. (2013). Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. The Lancet, 382(9901), 1329-1340.
Freire, G., & Karina, S. (2015). Ejercicios de buerguer allen en pacientes de 40 a 70 años que presentan venas varicosas grado 1 y 2 que acuden al centro eco-laser de varices y úlceras e Instituto de Trombosis Benalcázar en la ciudad de Latacunga (Bachelor's thesis, Universidad Técnica de Ambato-Facultad de Ciencias de la Salud-Carrera de Terapia Física).
Giacomozzi, C., D'Ambrogi, E., Cesinaro, S., Macellari, V., & Uccioli, L. (2008). Muscle performance and ankle joint mobility in long-term patients with diabetes. BMC musculoskeletal disorders, 9(1), 99.
Gisolf, J. (2005). Postural changes in humans: effects of gravity on the circulation.
Hanum, N. N. (2013). Hubungan Kadar Glukosa Darah Puasa dengan Profil Lipid pada Pasien Diabetes Melitus Tipe 2 di Rumah Sakit Umum Daerah Kota Cilegon Periode Januari 2012-April 2013.
Kementerian Kesehatan Republik Indonesia. (2014). Pusat data dan informasi Kementerian Kesehatan Republik Indonesia. Diakses dari: https://www.kemkes.go.id/resources/download/pusdatin/infodatin/infodatin-asi.pdf
Kementerian Kesehatan Republik Indonesia. (2013). Diabetes melitus penyebab kematian nomor 6 di dunia. Diakses dari: https://www.kemkes.go.id/article/view/2383/diabetes-melitus-penyebab-kematian-nomor-6-di-dunia-kemenkes-tawarkan-solusi-cerdik-melalui-posbindu.html
Kementerian Kesehatan Republik Indonesia. (2013). Riset Kesehatan Dasar 2013. Jakarta: Kementerian Kesehatan RI. Diakses dari: http://kesga.kemkes.go.id/images/pedoman/Data%20Riskesdas%202013.pdf
Kurniawan, I. (2010). Diabetes melitus tipe 2 pada usia lanjut. Majalah Kedokteran Indonesia, 60(12), 576-584.
Lestari, D. D. (2014). Gambaran Kadar Glukosa Darah Puasa Pada Mahasiswa Angkatan 2011 Fakultas Kedokteran Universitas Sam Ratulangi Dengan Indeks Massatubuh 18, 5-22, 9 Kg/m2. Jurnal e-Biomedik, 1(2).
Lord, S. R., Castell, S., Corcoran, J., Dayhew, J., Matters, B., Shan, A., & Williams, P. (2003). The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: a randomized, controlled trial. Journal of the American Geriatrics Society, 51(12), 1685-1692.
Malik, M., Bakir, A., Saab, B. A., Roglic, G., & King, H. (2005). Glucose intolerance and associated factors in the multi-ethnic population of the United Arab Emirates: results of a national survey. Diabetes research and clinical practice, 69(2), 188-195.
Ndraha, S. (2014). Diabetes melitus tipe 2 dan tatalaksana terkini. Medicinus, 27(2), 9-16.
Nurarif, A. H., & Kusuma, H.,(2015). Nanda Nic-Noc: asuhan keperawatan berdasarkan diagnose medis. Jakarta: Edisi Revisi jilid, 1.
Perkumpulan Endokrinologi Indonesia (2015), Penatalaksanaan DM Sesuai Konsesnsus Perkeni 2015 Https://Www.Academia.Edu/34970845/Penatalaksanaan_DM_Sesuai_Konsesnsus_Perkeni_2015 Diakses Pada tanggal 15 Desember 2018.
Roglic, G., Unwin, N., Bennett, P. H., Mathers, C., Tuomilehto, J., Nag, S., & King, H. (2005). The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes care, 28(9), 2130-2135.
Setiawan, B. (2017). Pengaruh program pengelolaan penyakit kronis (prolanis) terhadap tekanan darah pada pasien diabetes mellitus tipe II di Puskesmas Banjardawa (Doctoral dissertation, Muhammadiyah University of Semarang).
Shita, A. D. P. (2015). Perubahan level tnf-α il-1 pada kondisi diabetes mellitus.
Suominen, V., Uurto, I., Saarinen, J., Venermo, M., & Salenius, J. (2010). PAD as a risk factor for mortality among patients with elevated ABI–a clinical study. European Journal of Vascular and Endovascular Surgery, 39(3), 316-322.
Takahashi, T., Hayano, J., Okada, A., Saitoh, T., & Kamiya, A. (2005). Effects of the muscle pump and body posture on cardiovascular responses during recovery from cycle exercise. European journal of applied physiology, 94(5-6), 576-583.
Wikström, J., Hansen, T., Johansson, L., Lind, L., & Ahlström, H. (2008). Ankle brachial index< 0.9 underestimates the prevalence of peripheral artery occlusive disease assessed with whole-body magnetic resonance angiography in the elderly. Acta Radiologica, 49(2), 143-149.
Wilkinson, J. M., & Ahern, N. R. (2011). Buku saku diagnosis keperawatan. EGC.
DOI: https://doi.org/10.33024/hjk.v14i2.2742
Refbacks
- There are currently no refbacks.
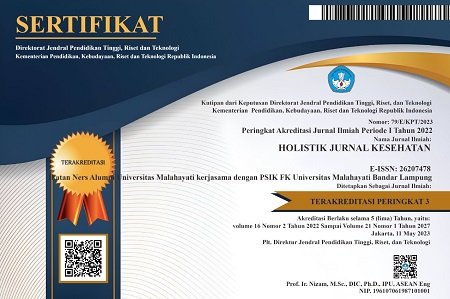
Copyright (c) 2020 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.