Pelaksanaan discharge planning pada pasien diabetes melitus: Studi literatur
Abstract
Background: Several studies have stated that patients with diabetes mellitus who do not get proper management when discharge after hospitalization are very at risk to readmission because of complications. Properly discharge planning programme is very essentials to reduce the number of readmission and following by controlled on patient's conditions. However, the fruitfulness level of discharge planning program in each hospital was different. planning in DM patients is still not optimal and does not explain in detail the discharge planning stages.
Purpose: To determine several studies of discharge planning programme among patients with diabetes mellitus in several hospital
Method: Literature study method with narrative review approach. Search for articles using databases by Science Direct, Pubmed and Google Scholar by entering keywords "discharge planning or return planning, Stages or steps, Diabetes or glycemic." From the search results, there were 13,743 articles that matched the keywords, then an examination carried out based on inclusion criteria (published year 2011-2020, articles in Indonesian and English, using the retrospect cohort method, RCT, and Quasi Experiment, full-text articles, discuss discharge planning stages) and exclusion criteria (articles on systematic reviews, proceedings, editorials and books). An examination carried out based on the title, sample, research method, and getting 10 articles.
Results: Analyzing result of 10 articles found that the discharge planning stage was the first stage starting from the time when admitting to hospital by conducting an assessment, diagnosis, planning, implementation and evaluation. The second stage was for the patient treated by providing education and training. Providing education included information about disease, signs and symptoms of disease, things that must avoid from experienced health problems and complications, and information about health service sources in the community. While training included the use of drugs, insulin, diet, physical activity, management of hypo and hyperglycemia, foot care, and blood glucose control. The third stage was after the patient discharged from the hospital by following up in form of telephone counseling and visits to the patient's home. The result of this literature study can be used as learning material for further research and material in providing nursing care.
Keywords: Discharge planning; Hospital; Patients; Diabetes mellitus; Literature studyPendahuluan: Pasien DM yang tidak mendapatkan penatalaksanaan yang tepat sangat beresiko mengalami berbagai komplikasi. Beberapa penelitian menyebutkan pasien DM cenderung kembali menjalani rawat ulang setelah pulang dari rumah sakit akibat dari komplikasi. Discharge planning terbukti dapat mengurangi jumlah kunjungan ulang ke rumah sakit dengan keluhan yang sama dan bahkan dapat mengurangi tingkat komplikasi. Namun, untuk saat ini, pelaksanaan discharge planning pada pasien DM masih kurang optimal dan tidak secara rinci menjelaskan tentang tahapan discharge planning.
Tujuan: Untuk mengetahui tahapan dalam pemberian discharge planning pada pasien diabetes melitus.
Metode: Penelitian ini menggunakan metode studi literatur dengan pendekatan narrative review. Pencarian artikel menggunakan database yaitu Science Direct, Pubmed dan Google Scholar dengan memasukkan kata kunci yaitu “discharge planning or perencanaan pulang, Stages or tahapan, Diabetes or glycemic. Dari hasil pencarian ditemukan sebanyak 13,743 artikel yang sesuai dengan kata kunci, kemudian dilakukan pemeriksaan berdasarkan kriteria inklusi (terbit tahun 2011-2020, artikel dalam Bahasa Indonesia dan Bahasa Inggris, menggunakan metode kohort retrospekti, RCT, dan Quasi Experiment, artikel tersedia full text, membahas tahapan discharge planning) serta kriteria eksklusi (Artikel systematic review, proceeding, editorial dan buku). Selanjutnya dilakukan pemeriksaan berdasarkan judul, sampel, metode penelitian, dan isi sehingga didapatkan 10 artikel.
Hasil: Dari 10 artikel ditemukan tahapan discharge planning tahap pertama dimulai sejak pasien masuk ke rumah sakit dengan melakukan pengkajian, diagnosa, perencanaan, implementasi, dan evaluasi. Tahap kedua selama pasien di rawat dengan memberikan pendidikan dan pelatihan. Pemberian pendidikan meliputi informasi tentang penyakit, tanda dan gejala penyakit, hal-hal yang harus dihindarkan dari gangguan kesehatan yang dialami dan komplikasi, serta informasi tentang sumber-sumber pelayanan kesehatan dimasyarakat. Sedangkan pelatihan meliputi penggunaan obat dan insulin, diet, aktivitas fisik, manajemen hipo dan hiperglikemia, perawatan kaki, dan kontrol glukosa darah. Tahap ketiga yaitu setelah pasien keluar dari rumah sakit dengan melakukan tindak lanjut berupa konseling telepon dan kunjungan ke rumah pasien. Hasil studi literatur ini dapat dijadikan sebagai bahan pembelajaran untuk penelitian selanjutnya dan bahan dalam memberikan asuhan keperawatan oleh perawat pada pasien diabetes melitus.
Keywords
References
Agustin, R. (2017). Optimalisasi pelaksanaan discharge planning melalui pengembangan model discharge planning terintegrasi pelayanan keperawatan. Jurnal Keperawatan Muhammadiyah. https://doi.org/10.30651/jkm.v2i1.921
Alloghani, M., Aljaaf, A., Hussain, A., Baker, T., Mustafina, J., Al-jumeily, D., & Khalaf, M. (2019). Implementation of machine learning algorithms to create diabetic patient re-admission profiles. BMC Medical Informatics and Decision Making, 19(Suppl 9), 1–16. https://doi.org/10.1186/s12911-019-0990-x
Amtsalina, A. (2016). Hubungan kepatuhan mengontrol gula darah dengan kejadian rawat inap ulang pasien diabetes melitus. (2014), 1–15.
Astuti, F., Suhartono, S., & Sulisno, M. (2016). Pengaruh ideal discharge planning terhadap kemampuan self care pasien diabetes melitus: studi pada pasien diabetes melitus di RSUD Kota Mataram Dan RSUD Provinsi NTB (Doctoral dissertation, Diponegoro University). http://eprints.undip.ac.id/47766/
Baethge, C., Goldbeck-wood, S., & Mertens, S. (2019). SANRA — a scale for the quality assessment of narrative review articles. 8, 2–8. https://doi.org/10.1186/s41073-019-0064-8
Darliana, D. (2012). Discharge planning dalam keperawatan Discharge Planning in Nursing ; A Literature Review. Idea Nursing Journal.
Dehnabi, A., Navipour, H., Radsepehr, H., & Tadayonfar, M. A. R. (2017). Effect of discharge planning on metabolic factors in type 2 diabetic patients. Journal of Client-Centered Nursing Care, 3(4), 251-262.. doi: 10.32598/jccnc.3.4.251
Dehnabi, A., Radsepehr, H., & Navipour, H. (2018). Evaluating the effect of discharge planning on glycosylated hemoglobin level in type 2 diabetic patients who referred to the Vasei Hospital in Sabzevar, Iran: An Interventional Study. Medical-Surgical Nursing Journal, 7(3).https://dx.doi.org/%2010.5812/msnj.87197
Daulay, M. (2018). Hubungan kadar HBA1C terhadap kadar glukosa darah puasa pada pasien penderita diabetes melitus tipe 2 di rumah Sakit Umum Pusat Haji Adam Malik. http://repositori.usu.ac.id/handle/123456789/10945
Demiris, G., Oliver, D. P., & Washington, K. T. (2019). Defining and analyzing the problem. Behavioral intervention research in hospice and palliative care, 27–39. https://doi.org/10.1016/b978-0-12-814449-7.00003-x
Federation, I. D. (2015). IDF Diabetes Atlas Seventh.
Fitri, E. Y., Andini, D., & Natosba, J. (2020). Effect of LIMA discharge planning model on discharge readiness a mong patients with diabetes mellitus. 25(Sicph 2019), 298–301. https://dx.doi.org/10.2991/ahsr.k.200612.041
Graham, J., Gallagher, R., & Bothe, J. (2013). Nurses' discharge planning and risk assessment: behaviours, understanding and barriers. Journal of clinical nursing, 22(15-16), 2338-2346.. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jocn.12179
Hardivianty, C. (2017). Evaluasi pelaksanaan discharge planning di Muhammadiyah Gamping Yogyakarta. 1(1), 21–34.
Jannah, N., Sukartini, T., & Hidayat, A. A. A. (2019). Discharge planning model with approach of method in improving patients’ readiness for discharge in hospitals. Indian Journal of Public Health Research & Development, 10(1). doi: 10.5958/0976-5506.2019.00057.3
Magny-Normilus, C., Nolido, N. V., Borges, J. C., Brady, M., Labonville, S., Williams, D., & Schnipper, J. L. (2019). Effects of an intensive discharge intervention on medication adherence, glycemic control, and readmission rates in patients with type 2 diabetes. Journal of patient safety. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7647006/
Natasia, N. (2017). Hubungan antara faktor motivasi dan supervisi dengan kinetja perawat dalam pendokumentasian discharge planning di RSUD Gambitan Kota Kediri, Jurnal aplikasi Manajemen. 97(4), 393–403.
Nurhayati, T. (2011). Pengaruh perencanaan pulang (discharge planning) untuk menjaga kestabilan kadar gula darah pada pasien diabetes mellitus paska rawat inap di Yanmasum Paviliun Rspad Gatot Soebroto Jakarta. Riset Keperawatan.
Pujiastuti, E. (2016). Hubungan pengetahuan dan motivasi dengan kepatuhan diet pada pasien diabetes mellitus tipe ii di poliklinik penyakit dalam rsud dr. soehadi prijonegoro sragen.
Purwanti, N., Yusuf, A., & Suprajitno. (2016). Pengaruh discharge planning berbasis video dengan pendekatan family centered nursing terhadap kemampuan keluarga merawat klien skizofrenia. 204–213. https://doi.org/10.33086/jhs.v10i2.131
Puspita, F. A., & Rakhma, L. R. (2018). Hubungan lama kepesertaan prolanis dengan tingkat pengetahuan gizi dan kepatuhan diet pasien diabetes mellitus di puskesmas gilingan surakarta. Jurnal Dunia Gizi, 1(2), 101-111. https://doi.org/10.33085/jdg.v1i2.3076
Ramayanti, E. D., & Huda, Y. N. (2014). Pengaruh Discharge Planning Terhadap Kesiapan Pulang Pada Pasien Diabetes Melitus. Java Health Jounal, 1(2), 81-88.Jane, G., Galakher, R. & Bothe, J. (2013). Nurse Discharge Planning and Risk assessment: Behaviour, understanding and barrier. Journal of Clinical Nursing, ed: 22. Bl.
Rostami, Z., Abedi, H., & Kalyani, M. N. (2016). The evaluation of hospital discharge plan effects on the self-caring ability of the patients suffering type-2 diabetes: A randomized clinical trial. International Journal of Medical Research & Health Sciences, 5(2), 92-98.
Sumarni, T., & Gafar, A. (2019). Discharge Planning Terintegrasi Dalam Pelayanan Klien Diabetes Mellitus Di Ruang Rawat Inap Penyakit Dalam Rsud Solok Tahun 2017. 14(1), 63–70.
Suryadi, R. F. (2013). Hubungan peran educator perawat dalam discharge planning dengan tingkat kepatuhan pasien rawat inap untuk kontrol di Rumah Sakit Paru Kabupaten Jember. http://repository.unej.ac.id/handle/123456789/3285
Suzuki, V. F., Carmona, E. V., & Lima, M. H. M. (2011). Planning the hospital discharge of patients with diabetes: the construction of a proposal. Revista Da Escola de Enfermagem Da USP., 2011; 45(2):515-20. doi: https://doi.org/10.1590/S0080-62342011000200032.
Soegondo, S., Soewondo, P., & Subekti, I. (2013). Penatalaksanaan Diabetes Melitus Terpadu. Edisi ke 2.
Tage, P. K. S., Novieastari, E., & Suhendri, A. (2018). Optimalisasi Pelaksanaan Discharge Planning Terstruktur Dan Terintegrasi. Chmk Nursing Scientific Journal, 2(April).
Taharuddin, T. (2017). Efektifitas Pelaksanaan Model Konservasi Discharge Planning Terstruktur Terhadap Perubahan Derajat Luka Dan Kadar Glukosa Darah Pada Pasien Ulkus Diabetikum. Care: Jurnal Ilmiah Ilmu Kesehatan, 5(3), 403-417. doi: https://dx.doi.org/10.33366/cr.v5i3.708
Wexler, D. J., Beauharnais, C. C., Regan, S., Nathan, D. M., Cagliero, E., Larkin, M. E., & Cde, M. S. R. N. (2012). Impact of inpatient diabetes management, education, and improved discharge transition on glycemic control 12 months after discharge. Diabetes Res Clin Pract, 98(2), 249–256. doi: https://doi.org/10.1016/j.diabres.2012.09.016.Impact
Wu, Y., Ding, Y., Tanaka, Y., & Zhang, W. (2014). Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. International Journal of Medical Sciences, 11(11), 1185. doi: 10.7150/ijms.10001.
World Health Organization [WHO]. (2016a). Diabetes facts, 1–2. doi: https://doi.org/10.1097/00152193-198704000-00001
World Health Organization [WHO]. (2016b). Global Report on Diabetes. Isbn, 978, 88. https://doi.org/ISBN 978 92 4 156525 7
Wrobleski, D.M.S. et al. (2014). Discharge Planning Rounds to the Bedside : A Patient- and Family- Centered Approach. , 23(2).
Zahroh, R., & Azkiyawati, M. (2015). Penerapan diabetes self management education meningkatkan pengetahuan, sikap dan pengendalian glukosa darah (Diabetes Self Management Education (DSME) toward Knowledge-Attitude and Control Blood Glucose). Journals of Ners Community, 6(2), 107-114. http://journal.unigres.ac.id/index.php/JNC/article/view/42/420
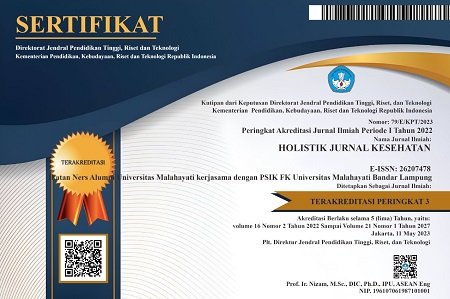
DOI: https://doi.org/10.33024/hjk.v14i4.3446
Refbacks
- There are currently no refbacks.
Copyright (c) 2020 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.