Pengetahuan kepala rumah tangga tentang Third-Hand Smoke (THS) dan keluhan pernapasan pada anak
Abstract
Background: Third-hand smoke (THS) is very dangerous, especially for children because of its content, properties, and the ability to last a long time on the surface of objects for months. Parents or families do not seem to care and know this hidden danger since they think as long as they do not smoke in front of their children, it means there is no problem.
Purpose: To identify the householder knowledge regarding third-hand tobacco smoke exposure and respiratory complaints in children
Method: This descriptive survey research with a cross-sectional approach was carried from August to November 2020 with householders of active smokers. The sampling technique was cluster sampling with a sample size of 561 respondents. The research instrument used the "Parent and Family Behavior Questionnaire against THS". Descriptive data analysis using SPSS 20 for Windows.
Results: Most of householders with active smokers had poor knowledge of THS by 451 respondents (80.4%), respiratory complaints in children were reported in 475 (84.7%) cases and the correlation between knowledge of householders about THS and respiratory complaints in children obtained p-value 0.000
Conclusion: Most of householders with active smokers had poor level of knowledge about THS and a significant relationship with respiratory complaints in children
Keywords: Knowledge; Householder; Third-Hand Smoke; Respiratory Complaints; ChildrenPendahuluan: Third-hand smoke (THS) sangatlah berbahaya terutama bagi anak-anak karena kandungan, sifat dan kemampuan bertahan lama pada permukaan benda hingga berbulan-bulan. Orang tua ataupun keluarga tampaknya tidak cukup peduli dan mengetahui bahaya tersembunyi ini sejak mereka menganggap selama tidak merokok di depan anak, itu berarti tidak ada masalah.
Tujuan: Untuk mengidentifikasi pengetahuan kepala rumah tangga tentang paparan THS dan keluhan pernapasan pada anak-anak
Metode: Penelitian survei deskriptif dengan pendekatan cross sectional ini dilakukan pada bulan Agustus hingga November 2020 terhadap kepala rumah tangga yang merupakan perokok aktif. Teknik pengambilan sampel adalah cluster sampling dengan jumlah sampel 561 responden. Instrumen penelitian menggunakan “Kuesioner Perilaku Orang Tua dan Keluarga Terhadap THS”. Analisis data deskriptif menggunakan SPSS 20 for Windows.
Hasil: Sebagian besar kepala rumah tangga perokok aktif memiliki pengetahuan buruk tentang THS sebesar 451 responden (80.4%), keluhan pernapasan pada anak dilaporkan terdapat 475 (84.7%) kasus dan korelasi antara pengetahuan kepala rumah tangga tentang THS dengan keluhan pernapasan pada anak diperoleh p-value 0.000
Simpulan: Sebagian besar kepala rumah tangga yang merupakan perokok aktif memiliki tingkat pengetahuan buruk tentang THS dan memiliki hubungan yang signifikan dengan keluhan pernapasan pada anak
Keywords
References
Acuff, L., Fristoe, K., Hamblen, J., Smith, M., & Chen, J. (2016). Third-Hand Smoke: Old Smoke, New Concerns. Journal of Community Health, 41(3), 680–687. https://doi.org/10.1007/s10900-015-0114-1
Agustin, H. (2019). Peningkatan awareness kerugian ekonomi akibat merokok pada warga ponegaran desa jambidan, kecamatan banguntapan, kabupaten Bantul. Jurnal Pemberdayaan: Publikasi Hasil Pengabdian Kepada Masyarakat, 3(1), 31-38.
Badan Penelitian dan Pengembangan Kesehatan Kementerian Kesehatan Republik Indonesia. (2015). Kerugian Negara Akibat Rokok Tahun 2015.
Ballantyne, C. (2009). What is third-hand smoke? Is it hazardous?. SCI. AM., January, 6.
Becquemin, M. H., Bertholon, J. F., Bentayeb, M., Attoui, M., Ledur, D., Roy, F., & Dautzenberg, B. (2010). Third-hand smoking: indoor measurements of concentration and sizes of cigarette smoke particles after resuspension. Tobacco Control, 19(4), 347–348. https://doi.org/10.1136/tc.2009.034694
Burton, A. (2011). Does the Smoke Ever Really Clear? Thirdhand Smoke Exposure Raises New Concerns. Environmental Health Perspectives, 119(2), A70-74. https://doi.org/10.1289/ehp.119-a70
Chao, M. R., Cooke, M. S., Kuo, C. Y., Pan, C. H., Liu, H. H., Yang, H. J., & Hu, C. W. (2018). Children are particularly vulnerable to environmental tobacco smoke exposure: Evidence from biomarkers of tobacco-specific nitrosamines, and oxidative stress. Environment International, 120(110), 238–245. https://doi.org/10.1016/j.envint.2018.08.006
Direktorat Pencegahan dan Pengendalian Penyakit Tidak Menular Kementerian Kesehatan Republik Indonesia. (2018). Indonesia sebagai Negara penghasil tembakau terbesar keenam. Retrieved from www.p2ptm.kemkes.go.id
Drehmer, J. E., Ossip, D. J., Nabi-Burza, E., Rigotti, N. A., Hipple, B., Woo, H., & Winickoff, J. P. (2014). Thirdhand Smoke Beliefs of Parents. Pediatrics, 133(4), e850-856. https://doi.org/10.1542/peds.2013-3392
Drehmer, J. E., Ossip, D. J., Rigotti, N. A., Nabi-Burza, E., Woo, H., Wasserman, R. C., Winickoff, J. P. (2012). Pediatrician interventions and thirdhand smoke beliefs of parents. American Journal of Preventive Medicine, 43(5), 533–536. https://doi.org/10.1016/j.amepre.2012.07.020
Escoffery, C., Bundy, L., Carvalho, M., Yembra, D., Haardörfer, R., Berg, C., & Kegler, M. C. (2013). Third-hand smoke as a potential intervention message for promoting smoke-free homes in low-income communities. Health Education Research, 28(5), 923–930. https://doi.org/10.1093/her/cyt056
Ferrante, G., Simoni, M., Cibella, F., Ferrara, F., Liotta, G., Malizia, V., & La Grutta, S. (2013). Third-hand smoke exposure and health hazards in children. Monaldi Archives for Chest Disease, 79(1), 38–43. https://doi.org/10.4081/monaldi.2013.108
Jacob III, P., Benowitz, N. L., Destaillats, H., Gundel, L., Hang, B., Martins-Green, M., & Whitehead, T. P. (2017). Thirdhand smoke: new evidence, challenges, and future directions. Chemical research in toxicology, 30(1), 270-294.
Kementerian Kesehatan Republik Indonesia. (2018). Hasil Utama Riset Kesehatan Dasar. https://doi.org/1
Kementerian Kesehatan Republik Indonesia. (2018). Situasi Umum Konsumsi Tembakau di Indonesia. Pusat Data dan Informasi Kementerian Kesehatan RI. Retrieved from file:///D:/infodatin tembakau per halaman.pdf
Mahabee-Gittens, E. M., Merianos, A. L., & Matt, G. E. (2018). Preliminary evidence that high levels of nicotine on children’s hands may contribute to overall tobacco smoke exposure. Tobacco Control, 27(2), 217–219. https://doi.org/10.1136/tobaccocontrol-2016-053602
Matt, G. E., Quintana, P. J. E., Hovell, M. F., Bernert, J. T., Song, S., Novianti, N., & Larson, S. (2004). Households contaminated by environmental tobacco smoke: Sources of infant exposures. Tobacco Control, 13(1), 29–37. https://doi.org/10.1136/tc.2003.003889
Matt, G. E., Quintana, P. J., Destaillats, H., Gundel, L. A., Sleiman, M., Singer, B. C., & Hovell, M. F. (2011). Thirdhand tobacco smoke: emerging evidence and arguments for a multidisciplinary research agenda. Environmental health perspectives, 119(9), 1218-1226.
Merritt, T. A., Mazela, J., Adamczak, A., & Merritt, T. (2012). The impact of second-hand tobacco smoke exposure on pregnancy outcomes, infant health, and the threat of third-hand smoke exposure to our environment and to our children. Przegląd Lekarski, 69(10), 717–720. Retrieved from http://www.wple.net/plek/numery_2012/numer-10-2012/717-720.pdf
Northrup, T. F., Khan, A. M., Jacob, P., Benowitz, N. L., Hoh, E., Hovell, M. F., & Stotts, A. L. (2016). Thirdhand smoke contamination in hospital settings: Assessing exposure risk for vulnerable pediatric patients. Tobacco Control, 25(6), 619–623. https://doi.org/10.1136/tobaccocontrol-2015-052506
Northrup, T. F., Matt, G. E., Hovell, M. F., Khan, A. M., & Stotts, A. L. (2016). Thirdhand smoke in the homes of medically fragile children: Assessing the impact of indoor smoking levels and smoking bans. Nicotine and Tobacco Research, 18(5), 1290–1298. https://doi.org/10.1093/ntr/ntv174
Öberg, M., Jaakkola, M. S., Woodward, A., Peruga, A., & Prüss-Ustün, A. (2011). Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. The Lancet, 377(9760), 139–146. https://doi.org/10.1016/S0140-6736(10)61388-8
Ott, W., Klepeis, N., & Switzer, P. (2008). Air change rates of motor vehicles and in-vehicle pollutant concentrations from secondhand smoke. Journal of Exposure Science and Environmental Epidemiology, 18(3), 312–325. https://doi.org/10.1038/sj.jes.7500601
Protano, C., & Vitali, M. (2011). The new danger of thirdhand smoke: Why passive smoking does not stop at secondhand smoke. Environmental Health Perspectives, 119(10), 422. https://doi.org/10.1289/ehp.1103956
Rabin, R. C. (2009). A New Cigarette Hazard : ’ Third-Hand Smoke ’. The New York Times, pp. 1–2.
Rehan, V. K., Sakurai, R., & Torday, J. S. (2011). Thirdhand smoke: A new dimension to the effects of cigarette smoke on the developing lung. American Journal of Physiology - Lung Cellular and Molecular Physiology, 301(1), 1–8. https://doi.org/10.1152/ajplung.00393.2010
Silaban, M. W. (2019). Hasil Litbang: Kerugian Pemerintah Akibat Rokok Rp 4.180 T. TEMPO.CO, pp. 4–5. Retrieved from https://bisnis.tempo.co/read/1223531/hasil-litbang-kerugian-pemerintah- akibat-rokok-rp-4-180-t/full&view=ok
Sleiman, M., Gundel, L. A., Pankow, J. F., Jacob, P., Singer, B. C., & Destaillats, H. (2010). Formation of carcinogens indoors by surface-mediated reactions of nicotine with nitrous acid, leading to potential thirdhand smoke hazards. Proceedings of the National Academy of Sciences, 107(15), 6576–6581. https://doi.org/10.1073/pnas.0912820107
Southeast Asia Tobacco Control Alliance. (2016). Indonesia , Negara dengan Jumlah Perokok Terbanyak di Asean.
Thomas, J. L., Hecht, S. S., Luo, X., Ming, X., Ahluwalia, J. S., & Carmella, S. G. (2014). Thirdhand tobacco smoke: A tobacco-specific lung carcinogen on surfaces in smokers’ homes. Nicotine and Tobacco Research, 16(1), 26–32. https://doi.org/10.1093/ntr/ntt110
United States. Public Health Service. Office of the Surgeon General. (2006). The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. US Department of Health and Human Services, Public Health Service, Office of the Surgeon General.
Winickoff, J. P., Friebely, J., Tanski, S. E., Sherrod, C., Matt, G. E., Hovell, M. F., & McMillen, R. C. (2009). Beliefs About the Health Effects of “Thirdhand” Smoke and Home Smoking Bans. Pediatrics, 123(1), e74–e79. https://doi.org/10.1542/peds.2008-2184
World Health Organization. (2017). WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies. Geneva: World Health Organization. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/255874/9789241512824-eng.pdf;jsessionid=AEE770B121C55D3353B9BD383AFAF65E?sequence=1
World Health Organization. (2018). WHO global report on trends in prevalence of tobacco smoking 2000-2025 (2nd ed.). Geneva: World Health Organization. Retrieved from http://apps.who.int/iris.
DOI: https://doi.org/10.33024/hjk.v15i2.3526
Refbacks
- There are currently no refbacks.
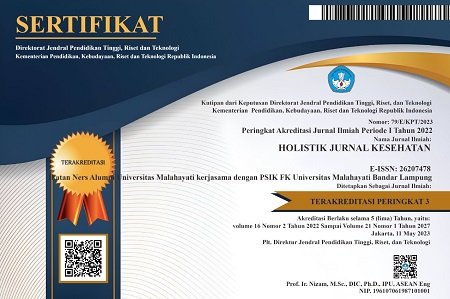
Copyright (c) 2021 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.