Studi literatur: Gambaran penerimaan diri penderita diabetes mellitus tipe II
Abstract
Background: Diabetes mellitus is a chronic disease that is a world health problem. Every year there is an increase in the number of morbidity that can be at risk of complications. DM patients require lifelong management to prevent complications. There is a change in lifestyle that can lead to feelings of hopelessness, so it is very important for sufferers to have an attitude of acceptance of illness. Low acceptance of illness can affect sufferers of poor disease management.
Purpose: To describe of acceptance of illness among patients with type 2 diabetes mellitus.
Method: Using published narrative artarticle obtained from a database-based search process. The data used are secondary data taken from national and international scientific articles starting from 2010 to 2020. The search engine used is Google Scholar and a database from PubMed. Analyzing keywords according to the topic, “acceptance of disease” OR “acceptance” OR “receiving” AND Diabetes mellitus OR Diabetes mellitus Type II.
Results: Finding was 10 articles showed 6 articles with a low level patient's acceptance of their illness which could affect sufferers such as low self-care, poor glycemic control, anxiety, depression, quality of life, emotional aspects and disrupting medication adherence while 4 articles showed high acceptance of illness showing DM management. adequate coping, low depression pressure, adherence to medication, good glycemic control and excellent quality of life.
Conclusion: The description of the patient's acceptance of their illness shows the results of all articles that developed and developing countries do not affect the acceptance of illness level. Of the 10 articles, 6 articles showed low acceptance of illness and 4 articles showed high acceptance of illness.
Keywords: Acceptance of illness; Patient; Type 2 diabetes mellitus
Pendahuluan: Diabetes Mellitus merupakan penyakit kronis yang menjadi masalah kesehatan dunia, setiap tahun mengalami peningkatan angka kesakitan yang dapat beresiko terjadi komplikasi. Pasien DM memerlukan pengelolaan seumur hidup untuk mencegah terjadi komplikasi. Terjadi perubahan pola hidup dapat menimbulkan rasa putus asa sehingga penting sekali penderita memiliki sikap acceptance of illness. Acceptance of illness yang rendah dapat mempengaruhi penderita terhadap managemen penyakit yang buruk
Tujuan: Mengetahui gambaran penerimaan diri penderita Diabetes Mellitus Tipe II
Metode: Menggunakan Narrative review artikel yang terpublikasi yang didapatkan dari proses pencarian berbasis database. Data yang digunakan yaitu data sekunder yang diambil dari artikel ilmiah nasional maupun internasional di mulai dari tahun 2010-2020. Search Engine yang digunakan adalah Google Schoolar dan database dari PubMed. Menganalisis kata kunci yang sesuai dengan topik, “penerimaan penyakit” ATAU “penerimaan” ATAU “menerima” DAN Diabetes Mellitus ATAU Diabetes Mellitus Tipe II
Hasil: Dari 10 artikel menunjukan 6 artikel dengan acceptance of illness rendah yang dapat menimbulkan dampak pada penderita seperti rendah perawatan diri, kontrol glikemik buruk, kecemasan, depresi, kualitas hidup, aspek emosional dan menganggu kepatuhan pengobatan sedangkan 4 artikel menunjukan acceptance of illness tinggi menunjukan managemen DM koping adekuat, tekanan depresi yang rendah, patuh pengobatan, kontrol glikemik baik dan kualitas hidup baik.
Simpulan: Gambaran tentang Acceptance Of Illness pada Penderita Diabetes Mellitus menunjukan hasil dari semua artikel bahwa negara maju dan berkembang tidak mempengaruhi pada tingkat acceptance of illness. Dari 10 artikel yang didapatkan 6 artikel menunjukan acceptance of illness rendah dan 4 artikel menunjukan acceptance of illness tinggi.
Keywords
References
Adailton, J., Cristina, E., Souza, F. De, Gretel, A., Böschemeier, E., Cristina, C., Bezerra, H. S., Emanuela, E., & Cavalcante, L. (2018). Diagnosis of diabetes mellitus and living with a chronic condition : participatory study. 1–8.
Bertolin, D. C., Pace, A. E., Cesarino, C. B., De Cassia Helu Mendonça Ribeiro, R., & Ribeiro, R. M. (2015). Psychological adaptation to and acceptance of type 2 diabetes mellitus. ACTA Paulista de Enfermagem, 28(5), 440–446. https://doi.org/10.1590/1982-0194201500074
Colberg, S. R., Sigal, R. J., Fernhall, B., Regensteiner, J. G., Blissmer, B. J., Rubin, R. R., Chasan-Taber, L., Albright, A. L., & Braun, B. (2010). Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: Joint position statement. Diabetes Care, 33(12). https://doi.org/10.2337/dc10-9990
Esen, A. (2012). Acceptance of illness and related factors in turkish patients with diabetes. 40(10).
Fidelity, T., Dulmen, S. Van, Psych, M. A., & Brembo, E. A. (2018). An mHealth Intervention for Persons with Diabetes Type 2 Based on Acceptance and Commitment Therapy Principles : Examining Corresponding Author : 6, 1–17. https://doi.org/10.2196/mhealth.9942
Inonu, V. F., Srw, D. W., & Rodiani. (2018). Hubungan Penerimaan Diri Dengan Self-Management Diabetes Mellitus Pada Peserta Prolanis di Puskesmas Kedaton Bandarlampung The Relationship Between Self-Acceptance with Self-Management of Diabetes Mellitus on Prolanist Participants in Kedaton Health Cente. Keperawatan, 90–94.
Kapucu, S. (2019). Relationship between adherence to treatment and acceptance of illness in patients with type 2 diabetes Tip 2 diyabetli hastalarda tedaviye uyum ve hastalık kabulü arasındaki ilişki. December. https://doi.org/10.17826/cumj.554402
Khashouei, M. M., Ghorbani, M., & Tabatabaei, F. (2016). The Effectiveness of Acceptance and Commitment Therapy (ACT) on Self-Efficacy, Perceived Stress and Resiliency in Type II Diabetes Patients. Global Journal of Health Science, 9(5), 18. https://doi.org/10.5539/gjhs.v9n5p18
Richardson, A., Adner, N., & Nordström, G. (2001). Persons with insulin‐dependent diabetes mellitus: acceptance and coping ability. Journal of advanced nursing, 33(6), 758-763.
Rn, K. Z., Bruzzese, J. M., Smaldone, A., & Pc, C. (2019). Illness acceptance in adolescents : A concept analysis. Nursing Forum, 1–8. https://doi.org/10.1111/nuf.12368
Rogon, I., Kasprzak, Z., & Szcześniak, Ł. (2017). Perceived quality of life and acceptance of illness in people with type 2 diabetes mellitus. 16(3), 79–85.
Rumaiza, R., & Khairani, K. (2019). Faktor-faktor yang berhubungan dengan tingkat stres pada lansia penderita diabetes mellitus Tipe II di RSUD Banda Aceh. Jurnal Ilmiah Mahasiswa Fakultas Keperawatan, 4(2).
Salami, S. (2017). Faktor Sosiodemografi dan Self Efficacy Penderita Diabetes Mellitus Tipe 2 (Study pada Peserta Prolanis) di Puskesmas Talaga Bodas Bandung. Jurnal Medika Cendikia, 4(01), 58-66.
Schmitt, A., Reimer, A., Kulzer, B., Haak, T., Gahr, A., & Hermanns, N. (2014). Educational and psychological issues assessment of diabetes acceptance can help identify patients with ineffective diabetes self-care and poor diabetes control. Diabetic Medicine, 31(11), 1446–1451. https://doi.org/10.1111/dme.12553
Schmitt, Andreas, Reimer, A., Kulzer, B., Icks, A., Paust, R., Roelver, K., Kaltheuner, M., Ehrmann, D., Krichbaum, M., Haak, T., & Hermanns, N. (2018). Journal of Diabetes and Its Complications Measurement of psychological adjustment to diabetes with the diabetes acceptance scale. Journal of Diabetes and Its Complications, 32(4), 384–392. https://doi.org/10.1016/j.jdiacomp.2018.01.005
Shayeghian, Z. (2016). و ﻪﻠﯾزﻮﮑﯿﻠﮔ ﻦﯿﺑﻮﻠﮔﻮﻤﻫ دﻮﺒﻬﺑ ﺮﺑ ﺪﻬﻌﺗ و شﺮﯾﺬﭘ ﺮﺑ ﯽﻨﺘﺒﻣ ﯽﻧﺎﻣرد هوﺮﮔ ﯽﺸﺨﺑﺮﺛا ود عﻮﻧ ﺖﺑﺎﯾد ﻪﺑ نﺎﯾﻼﺘﺒﻣ رد ﯽﺘﺒﻗاﺮﻣدﻮﺧ يﺎﻫ ﺖﯿﻟﺎﻌﻓ Effectiveness of acceptance and commitment group therapy on improvement of glaycated hemoglobin and self-care activities in patients . 10(2), 41–50.
Shiyanbola, O. O., Unni, E., Huang, Y. M., & Lanier, C. (2018). Using the extended self-regulatory model to characterise diabetes medication adherence: A cross-sectional study. BMJ Open, 8(11), 1–9. https://doi.org/10.1136/bmjopen-2018-022803
Starczewska, M., Kujawska, R., & Stanisławska, M. (2018). The analysis of health behaviors and illness acceptance in patients with diabetes. 20(4), 352–355.
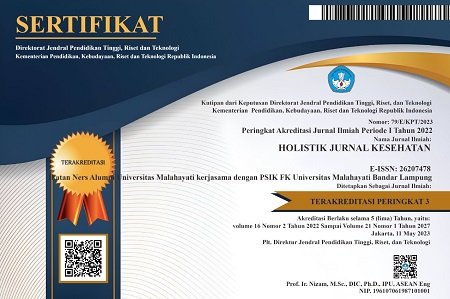
DOI: https://doi.org/10.33024/hjk.v15i1.4093
Refbacks
- There are currently no refbacks.
Copyright (c) 2021 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.