Faktor-faktor determinan penyebab loss to follow up pada orang dengan HIV dan AIDS (ODHA) yang menerima terapi Antiretroviral (ARV)
Abstract
Background: Based on data from the Tangerang District Hospital in October 2020, it was found that data on follow-up under antiretroviral therapy (ARV) among people living with HIV/AIDS (PLWHA) during the pandemic period for the last 3 months from February to April 2020 showed a decrease in the number but had a fluctuating graph in taking drugs every month, reaching 1012 patients, of which 20% were children. In addition, during the pandemic, there was an increase in LFU (lost to follow-up) cases of ARV treatment regimens.
Purpose: To identify determinant factors of loss to follow-up under antiretroviral therapy (ARV) among people living with HIV/AIDS (PLWHA)
Method: A quantitative research with a cross-sectional approach. The number of samples in this study was 45 respondents. The analysis used is univariate and bivariate. The statistical tests used are Chi-Square test and logistic regression.
Results: Finding that the factors related to the cause of the withdrawal of ARV drugs were health insurance, side effects of ARVs, CD4 values, family support, hopelessness, stress levels, and self-esteem. Then a logistic regression test was carried out to find out which factor had the most influence and the results showed that the CD4 value was the most significant indicator with an OR (Odds Ratio) value of 26,812 812, meaning that people living with HIV who had CD4 values < 200 had a 26,812 times greater risk of dropping out of ARV drugs, compared to people living with HIV who have CD4 values 200.
Conclusion: CD4 value is the most significant factor in the incidence of ARV drug withdrawal in living with HIV.
Keywords: Loss to follow-up; Antiretroviral therapy (ARV); People living with HIV/AIDS (PLWHA)
Pendahuluan: Berdasarkan data RSUD Kab.Tangerang Oktober 2020 didapatkan data follow up pada orang dengan HIV dan AIDS (ODHA) yang menerima terapi Antiretroviral (ARV selama masa pandemi 3 bulan terakhir Februari-April 2020 menunjukan penurunan angka follow up namum memiliki grafik fluktuatif dalam pengambilan obat tiap bulan mencapai 1012 pasien dimana 20% termasuk usia anak. Selain itu, selama pandemi terjadi peningkatan kasus LFU (lost to follow up) dari regiment pengobatan ARV.
Tujuan: Mengidentifikasi faktor-faktor determinan penyebab loss to follow up pada orang dengan HIV dan AIDS (ODHA) yang menerima terapi Antiretroviral (ARV)Metode: Penelitian kuantitatif dengan pendekatan cross sectional. Jumlah sampel dalam penelitian ini 45 responden. Analisis yang digunakan adalah univariat dan bivariat. Uji statistik yang digunakan yakni, uji Chi Square dan regresi logistik.
Hasil: Didapatkan bahwa faktor yang berhubungan dengan penyebab loss to follow up ARV adalah jaminan kesehatan, efek samping ARV, nilai CD4, dukungan keluarga, keputusasaan, tingkat stress, dan harga diri. Selanjutnya dilakukan uji regresi logistic untuk mendapatkan faktor mana yang paling berpengaruh dan didapatkan hasil bahwa nila CD4 merupakan indicator paling bermakna dengan nilai OR (Odds Rasio) sebesar 26.812 812 artinya ODHA yang memiliki kadar nilai CD4 < 200 memiliki risiko 26.812 kali lebih besar penyebab loss to follow up ARV dibandingkan dengan ODHA yang memiliki kadar nilai CD4 ≥ 200.
Simpulan: Nilai CD4 merupakan faktor yang paling bermakna terhadap kejadian loss to follow up ARV pada ODHA.
Keywords
References
Alli, R. A. (2020). Children With HIV and AIDS. https://www.webmd.com/hiv-aids/guide/hiv-in-children
Astuti, D., & Mulyaningsih, M. (2016). Peran Perawat sebagai Educator Mempengaruhi Kepatuhan Konsumsi Obat Antiretroviral (ARV) Bagi Pasien HIV/AIDS di Klinik VCT RSUD Dr. Moewardi. Jurnal Ners Dan Kebidanan (Journal of Ners and Midwifery); Vol 3, No 3 (2016)DO - 10.26699/Jnk.V3i3.ART.P183-188 . https://jnk.phb.ac.id/index.php/jnk/article/view/0121
Ballivian, J., Alcaide, M. L., Cecchini, D., Jones, D. L., Abbamonte, J. M., & Cassetti, I. (2020). Impact of COVID-19-Related Stress and Lockdown on Mental Health Among People Living With HIV in Argentina. Journal of Acquired Immune Deficiency Syndromes (1999), 85(4), 475–482. https://doi.org/10.1097/QAI.0000000000002493
Baroya, N. M. (2017). Prediktor sikap stigma dan diskriminasi terhadap orang dengan HIV dan AIDS (ODHA) di Kabupaten Jember. Ikesma, 13(2).
Centers for Disease Control and Prevention. (2019). AIDS and Opportunistic Infections. https://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html
Cortes, A., Hunt, N., & McHale, S. (2014). Development of the scale of perceived social support in HIV (PSS-HIV). AIDS and Behavior, 18(12), 2274–2284. https://doi.org/10.1007/s10461-014-0902-0
Debby, C., Sianturi, S. R., & Susilo, W. H. (2019). Faktor-faktor yang berhubungan dengan kepatuhan minum obat ARV pada pasien hiv di RSCM Jakarta. J. UMM, 10(1).
Hakim, M. Z., Putra, I., & Heryana, W. (2019).
Keinginan bunuh diri orang dengan HIV dan Aids (ODHA) dampingan yayasan PKBI DKI Jakarta. Jurnal Ilmiah Rehabilitasi Sosial, 01(1), 93–110.
Harison, N., Waluyo, A., & Jumaiyah, W. (2020). Pemahaman pengobatan antiretroviral dan kendala kepatuhan terhadap terapi antiretroviral pasien HIV/AIDS. JHeS (Journal of Health Studies), 4(1), 87-95.
Heywood, W., & Lyons, A. (2016). HIV and Elevated Mental Health Problems: Diagnostic, Treatment, and Risk Patterns for Symptoms of Depression, Anxiety, and Stress in a National Community-Based Cohort of Gay Men Living with HIV. AIDS and Behavior, 20(8), 1632–1645. https://doi.org/10.1007/s10461-016-1324-y
Kalalo, J. G., Tjitrosantoso, H., & Goenawi, L. R. (2012). Studi penatalaksanaan terapi pada penderita HIV/AIDS di klinik VCT rumah sakit kota Manado. Pharmacon, 1(2).
Karyadi, T. H. (2017). Keberhasilan Pengobatan Antiretroviral (ARV). Jurnal Penyakit Dalam Indonesia, 4(1). http://www.jurnalpenyakitdalam.ui.ac.id/index.php/jpdi/article/viewFile/105/95
Kementerian Kesehatan Republik Indonesia. (2014). Pedoman penerapan terapi hiv pada anak. World Health Organization, 1–81. Diakses dari: https://spesialis1.ika.fk.unair.ac.id/wp-content/uploads/2017/03/Pedoman-Penerapan-Terapi-HIV-pada-Anak-1.pdf
Kementerian Kesehatan Republik Indonesia. (2019). Hari HIV/AIDS Sedunia, Penanganan Diperkuat di Daerah. diakses dari: https://www.kemkes.go.id/article/view/19112900001/hari-hiv-aids-sedunia-penanganan-diperkuat-di-daerah.html
Latipah, S., & Milanda, C. (2021). The Relationship of Social Stigma and Quality Of Life in Children with. Journal Center of Research Publication in Midwifery and Nursing, 5, 31–39. https://ejournal.binausadabali.ac.id/index.php/caring/article/view/201
Liamputtong, P. (2016). Children, young people and HIV/AIDS: a cross-cultural perspective. In Children and Young People Living with HIV/AIDS (pp. 1-20). Springer, Cham. https://doi.org/10.1007/978-3-319-29936-5_1
Mahajan, A. P., Sayles, J. N., Patel, V. A., Remien, R. H., Ortiz, D., Szekeres, G., & Coates, T. J. (2008). Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS (London, England), 22(Suppl 2), S67. https://doi.org/10.1097/01.aids.0000327438.13291.62
Manhas, C. (2014). Self-esteem and quality of life of people living with HIV/AIDS. Journal of Health Psychology, 19(11), 1471–1479. https://doi.org/10.1177/1359105313493812
Mukarromah, S., & Azinar, M. (2021). Penghambat Kepatuhan Terapi Antiretroviral Pada Orang Dengan HIV/AIDS (Studi Kasus Pada ODHA Loss To Follow Up Therapy). Indonesian Journal of Public Health and Nutrition, 1(3), 396-406.
Naif, H. M. (2013). Pathogenesis of HIV Infection. Infectious Disease Reports, 5(Suppl 1), e6–e6. https://doi.org/10.4081/idr.2013.s1.e6
Phillips, H. (2022). HIV prevention essential for ending generalised epidemics, despite test and treat Retrieved from https://www.beintheknow.org/news-and-blogs/hiv-prevention-essential-ending-generalised-epidemics-despite-test-and-treat
Pinquart, M. (2013). Self‐esteem of children and adolescents with chronic illness: a meta‐analysis. Child: care, health and development, 39(2), 153-161. https://doi.org/10.1111/j.1365-2214.2012.01397.x
Rahakbauw, N. (2016). Dukungan Keluarga Terhadap Kelangsungan Hidup ODHA (orang dengan HIV/AIDS). Insani Jurnal, 3(2).
Riwayati, R., & Hidayati, E. (2015). Efektifitas Psikoedukasi terhadap Kemampuan Keluarga Merawat Anggota Keluarga Penderita HIV-AIDS di Wilayah Kota Semarang. Jurnal Keperawatan Jiwa (JKJ): Persatuan Perawat Nasional Indonesia, 3(1), 6-12.
Rumah Sakit Umum Daerah Kabupaten Tangerang. (2020). Data Kunjungan ODHA.
Sari, A. M. (2021). The Relationship between The Level of Side Effects of ARV Drugs in ODHA Patients to The Level of The Compliance Use of ARV Drugs. Pharmaceutical Journal of Indonesia, 6(2), 125-129. https://doi.org/10.21776/ub.pji.2021.006.02.8
Superkertia, I., Astuti, I., & Lestari, M. (2016). Hubungan Antara Tingkat Spiritualitas Dengan Tingkat Kualitas Hidup Pada Pasien Hiv/Aids Di Yayasan Spirit Paramacitta Denpasar. COPING NERS (Community of Publishing in Nursing), 4(1), 49–53. https://ojs.unud.ac.id/index.php/coping/article/view/14077
Yang, T. W., Park, H. O., Jang, H. N., Yang, J. H., Kim, S. H., Moon, S. H., Byun, J. H., Lee, C. E., Kim, J. W., & Kang, D. H. (2017). Side effects associated with the treatment of multidrug-resistant tuberculosis at a tuberculosis referral hospital in South Korea: A retrospective study. Medicine, 96(28), e7482–e7482. https://doi.org/10.1097/MD.0000000000007482
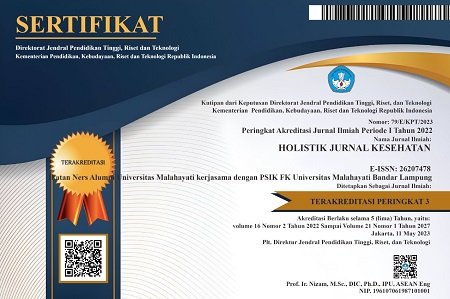
DOI: https://doi.org/10.33024/hjk.v16i6.7820
Refbacks
- There are currently no refbacks.
Copyright (c) 2022 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.