Hubungan dislipidemia dengan kejadian stroke
Abstract
Background: Stroke is a loss of brain function caused by the cessation of blood supply to part of the brain, which results in impaired blood flow to the brain and can cause blockage (ischemic stroke) or bleeding (hemorrhagic stroke). Dyslipidemia and hyperlipidemia are risk factors for stroke, which is a lipid profile disorder characterized by a decrease or increase. The main lipid profiles were total cholesterol levels, triglyceride levels, HDL-C levels, and LDL-C levels.
Purpose: To determine the relationship between cholesterol levels with ischemic (non-hemorrhagic) and hemorrhagic stroke
Method: A descriptive-analytic correlative observational study with a retrospective cross-sectional approach. The sampling technique using purposive sampling obtained as many as 30 samples. Processing and analysis of the data obtained using a program on a computer. Analysis of the data used is a univariate, bivariate, and multivariate analysis using contingency coefficients with a significance level of p <0.05.
Results: Most respondents have high total cholesterol levels as many as 24 respondents (80%), and high triglyceride levels as many as 19 respondents (63.3%). High LDL-C levels were 16 respondents (53.3%), and high HDL-C levels were 16 respondents (53.3%). Calculation of statistical tests obtained the results of total cholesterol levels p=0.033 (p<0.05), triglyceride levels p=0.016 (p<0.05), LDL-C levels p=0.464 (p>0.05), HDL levels -C p=0.088 (p>0.05). Multivariate analysis using multiple logistic regression was the most correlated of the characteristics of dyslipidemia with the incidence of stroke in total cholesterol levels (p = 0.014).
Conclusion: Dyslipidemia and dyslipidemia characteristics, namely total cholesterol and triglyceride levels have a significant relationship with the incidence of stroke. The most related characteristic of dyslipidemia is total cholesterol level with the incidence of stroke.
Keywords: Cholesterol level; Ischemic (non hemorrhagic); Hemorrhagic strokePendahuluan: Stroke adalah kehilangan fungsi otak yang diakibatkan oleh terhentinya suplai darah kebagian otak, yang mengakibatkan gangguan aliran darah ke otak dan dapat menyebabkan penyumbatan (ischemic stroke) atau pendarahan (hemorrhagic stroke). Dislipidemia dan hiperlipidemia adalah suatu faktor risiko stroke yang merupakan suatu kelainan profil lipid yang ditandai dengan adanya penurunan atau peningkatan. Profil lipid yang utama adalah kadar kolesterol total, kadar trigliserida, kadar HDL-C, dan kadar LDL-C.
Tujuan: Untuk mengetahui hubungan kadar kolesterol dengan stroke hemoragik and iskemik (non hemoragik).
Metode: Deskriptif analitik korelatif dengan pendekatan cross sectional yang bersifat retrospektif. Teknik pengambilan sampel dengan purposive sampling didapatkan sebanyak 30 sampel. Pengolahan dan analisis data yang diperoleh menggunakan program SPSS. Analisa data yang digunakan adalah analisa univariat, bivariat dan multivariat menggunakan koefisiensi kontigensi dengan tingkat kemaknaan p<0,05.
Hasil: Menunjukkan bahwa sebagian besar responden memiliki kadar total kolesterol tinggi sebanyak 24 reponden (80%), kadar trigliserida yang tinggi sebanyak 19 responden (63,3%), kadar LDL-C tinggi sebanyak 16 responden (53,3%), dan kadar HDL-C tinggi sebanyak 16 responden (53,3%). Perhitungan uji statistik diperoleh hasil kadar total kolesterol p=0,033 (p<0,05), kadar trigliserida p=0,016 (p<0,05), kadar LDL-C p=0,464 (p>0,05), dan kadar HDL-C p=0,088 (p>0,05). Analisis multivariat dengan menggunakan regresi logistic berganda yang paling berhubungan dari karakteristik dislipidemia dengan kejadian stroke ialah kadar total kolesterol (p=0,014).
Simpulan: Dislipidemia dan karakteristik dislipidemia yaitu kadar total kolesterol dan trigliserida memiliki hubungan yang bermakna dengan kejadian stroke. Karakteristik dislipidemia yang paling berhubungan yaitu kadar total kolesterol dengan kejadian stroke.
Keywords
References
Almatsier, S. (2015). Prinsip dasar ilmu gizi, PT. Gramedia Pustaka Utama, Jakarta. American Stroke Association, (2018). Stroke risk; the changes you make now make change what happen slater, 10 Maret 2018. http://www.strokeassociation.org/STROKEORG/AboutStroke/UnderstandingRisk/Understanding-Stroke-Risk_UCM_308539_SubHomePage.jsp
Corwin, E. J. (2018). Buku Saku Patofisiologi, ed 3 (ed Egi Komara Yuda et al). Jakarta. EGC
Freiberg, J. J., Tybjærg-Hansen, A., Jensen, J. S., & Nordestgaard, B. G. (2008). Nonfasting triglycerides and risk of ischemic stroke in the general population. Jama, 300(18), 2142-2152.
Goldberg, A. C., Leiter, L. A., Stroes, E. S., Baum, S. J., Hanselman, J. C., Bloedon, L. T., & Duell, P. B. (2019). Effect of bempedoic acid vs placebo added to maximally tolerated statins on low-density lipoprotein cholesterol in patients at high risk for cardiovascular disease: the CLEAR wisdom randomized clinical trial. Jama, 322(18), 1780-1788.
Hakim, R. A. S. (2013). Hubungan antara dislipidemia dengan kejadian stroke di bangsal rawat inap irna b 1 bagian neurologi Rumah Sakit Umum Pusat (RSUP) Dr. Kariadi Semarang (Doctoral dissertation, UNIMUS).
Harris, S., Kurniawan, M., Mesiano, T., Rasyid, A., & Hidayat, R. (2018).Cerebral small vessel diseasein Indonesia: Lacunar infarction study from Indonesian Stroke Registry 2012–2014. SAGE Open Medicine, Volume 6: 1 –6.
Imamura, T., Doi, Y., Arima, H., Yonemoto, K., Hata, J., Kubo, M., & Kiyohara, Y. (2009). LDL cholesterol and the development of stroke subtypes and coronary heart disease in a general Japanese population: the Hisayama study. Stroke, 40(2), 382-388.
Jamini, T., Yulyanti, Y., & Negara, C. K. (2020). Hubungan Kadar Kolesterol Darah dan Hipertensi dengan Kejadian Stroke Di RSUD Ulin Banjarmasin. Jurnal Kesehatan Indonesia, 11(1), 27-34.
Kementerian kesehatan Republik Indonesia. (2013). Pedoman pengendalian stroke. Jakarta: Direktorat Pengendalian Penyakit Tidak Menular. Available from: https://p2ptm.kemkes.go.id/dokumen-ptm/pedoman-pengendalian-stroke
Kementerian Kesehatan Republik Indonesia. (2013). Riset kesehatan dasar (Riskesdas) 2013. Kemenkes RI. Jakarta. Available from: http://www.badankebijakan.kemkes.go.id/laporan-hasil-riset-kesehatan-dasar-riskesdas/
Kementerian Kesehatan Republik Indonesia. (2014). Situasi dan Analisis Diabetes. https://www.kemkes.go.id/article/view/15021800007/situasi-dan-analisis-diabetes.html
Kementerian Kesehatan Republik Indonesia. (2018). Hasil Utama Riset kesehatan dasar (Riskesdas) 2018. Kementerian Kesehatan Republik Indonesia, Badan Penelitian dan Pengembangan Kesehatan. Available from: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf
Marlina, Y., (2011). Gambaran Factor Resiko Pada Penderita Stroke Iskemik Di RSUP H. Adam Malik Medan Tahun 2018. Medan : Fakultas Kedokteran Universitas Sumatra Utara; Available from URL: HIPERLINK http://repository.usu.ac.id/handle/123456789/31212 diunduh pada Sabtu 28 Februari 2021
Meschia, J. F., Bushnell, C., Boden-Albala, B., Braun, L. T., Bravata, D. M., Chaturvedi, S., & Wilson, J. A. (2014). Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 45(12), 3754-3832.
Misbach, J. (2011). Stroke aspek diagnostik, patofisiologi, manajemen. Jakarta: FKUI.
Prasetyo, E., & Garini, A. S. (2018). Prevalensi Dislipidemia pada Pasien Stroke Iskemik Berulang Rawat Jalan dan atau Rawat Inap di Rumah Sakit Pusat Otak Nasional Periode 2015 –Juni 2017. Majalah Kesehatan Pharmamedika, 10(1), 031-039.
Pratiwi, N. (2017). Hubungan antara profil lipid dengan kejadian stroke tahun 2016 di Rsud Wates Kulon Progo (Doctoral dissertation, STIKES Jenderal Achmad Yani Yogyakarta).
Pujarini, L. (2009). Dislipidemia pada Penderita Stroke dengan Demensia di RS Dr. Sardjito Jogjakarta.
Purnomo, R. T., Widjajanto, E., & Sulistyarini, I. (2017). Analisis Faktor-Faktor yang Mempengaruhi Kejadian Stroke Akut pada Pasien Stroke yang Dibawa ke Instalasi Gawat Darurat RSI Klaten. MOTORIK Jurnal Ilmu Kesehatan, 12(24).
Sastroasmoro, S., & Ismael, S. (2018). Dasar-dasar metodologi penelitian klinis Edisi ke-4. Jakarta: Sagung Seto, 376.
Soebroto, L. (2010). Hubungan antara kadar ldl kolesterol pada penderita stroke di rumah sakit Dr. Moewardi Surakarta.
Tirschwell, D. L., Smith, N. L., Heckbert, S. R., Lemaitre, R. N., Longstreth, W. T., & Psaty, B. M. (2004). Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups. Neurology, 63(10), 1868-1875. Availablefrom URL: HIPERLINK http://www.neurology.org/content/63/10/1868.abstract?ijke=9019d6f6b3bddd037ca0550f05bb7eb840c17f0e&keytype2=tf_ipsecs diunduh 26 Maret 2021
Wang, L., Cui, W., Nan, G., & Yu, Y. (2015). Meta-analysis reveals protective effects of vitamin B on stroke patients. Translational Neuroscience, 6(1), 150-156.
Wardaini, L., Listyaningrum, D., Surbakti, K. P., & Nasution, D. (2012). Hubungan trigliserida tidak puasa dengan kejadian stroke iskemik.
World Health Organization.(2017). Global Burden Of Stroke. World Health Organization; 2. Available from: URL: HIPERLINK http://www.who.int/cardiovascular_disease/en/cvd_atlas_15_burden_strok e.pdf, diunduh pada 23 Februari 2021.
Ying, C. Y., Harith, S., Ahmad, A., & Mukhali, H. B. (2018). Prevalence, Risk Factors And Secondary Prevention Of Stroke Recurrence In Eight Countries From South, East And Southeast Asia: A Scoping Review. Med J Malaysia Vol 73, 90-99.
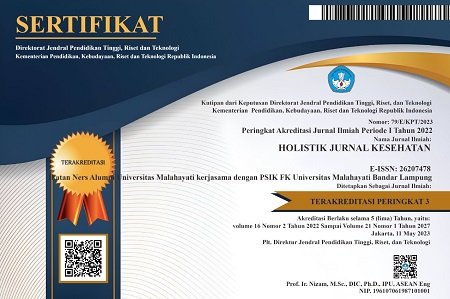
DOI: https://doi.org/10.33024/hjk.v16i6.8089
Refbacks
- There are currently no refbacks.
Copyright (c) 2022 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.