Analisis faktor pemanfaatan pelayanan Rumah Sakit Jiwa: Systematic literature review
Abstract
Background: Mental disorders are illnesses that have an impact on mood, behavior, thinking, or a combination of the three. In Indonesia, there are 236 million people who suffer from mental illnesses, with moderate mental disorders accounting for 6 percent of the population and severe mental illnesses for 0.17 percent of the population, 14.3 percent of whom are shackled. Up to 61.86 percent of individuals with mental illnesses lack access to basic medical care. This is due to the fact that Indonesia's access to mental health care has not been equal, high-quality, or cost-effective.
Purpose: Provide an overview of the factors that influence the use of mental hospital services.
Method: The Google Scholar, Scient Direct, Spinger, and Proquest databases were used to conduct article searches and were done between 2017 and 2022. The keywords "Utilization of mental hospital services" and "factors that influence mental hospital visits" were used in the article search. Additionally, inclusion and exclusion standards were used when looking for relevant research publications.
Results: The utilization of mental hospital services is influenced by several factors, those are: 1) The accessibility of mental health services throughout the world is not evenly distributed. 2) A family's willingness to accept a member who has a mental disorder will boost recovery; 3) A family's ability to deal with a member who has a mental disorder will be improved.4) The family that accompanies them to the mental hospital tends to be male; 5) Families with limited resources may not stick to treatment; and 6) The stigma of society, which results in stigmatization and social exclusion for those with mental illnesses.
Conclusion: Accessibility, attitude, knowledge, gender, financial support, and stigma are factors that affect the use of services at mental hospitals.
Keywords: Utilization; Patient; Mental Disorders; Mental Hospital.
Pendahuluan: Gangguan jiwa merupakan kondisi kesehatan yang berpengaruh terhadap pemikiran perilaku, suasana hati, atau kombinasi diantara ketiganya. Di Indonesia, jumlah penderita gangguan jiwa mencapai 236 juta orang, dengan kategori gangguan jiwa ringan 6 persen dari populasi dan 0,17 persen menderita gangguan jiwa berat, dimana 14,3 persen diantaranya mengalami pasung. Sebanyak 61,86 persen penderita gangguan jiwa belum mendapatkan akses layanan kesehatan sesuai dengan standar. Hal ini disebabkan karena kondisi akses pelayanan kesehatan jiwa di Indonesia belum memenuhi kebutuhan yang bermutu, terjangkau, dan merata.
Tujuan: Memberikan tinjauan akan faktor-faktor yang mempengaruhi pemanfaatan pelayanan rumah sakit jiwa.
Metode: Pencarian artikel dilakukan dengan menggunakan database Google Scholar, Scient Direct, Spinger, dan Proquest. Pencarian artikel dilakukan antara tahun 2017 sampai tahun 2022. Kata kunci yang digunakan dalam pencarian artikel yaitu dengan kata kunci “Utilization of mental hospital service” dan “factors that influence mental hospital visits”. Kriteria inklusi dan ekslusi juga diterapkan dalam pencarian artikel penelitian terkait.
Hasil: Pemanfaatan pelayanan rumah sakit jiwa dipengaruhi oleh beberapa faktor, yaitu: Aksesibilitas pelayanan kesehatan jiwa di seluruh dunia belum merata; Sikap positif keluarga dalam menerima anggota keluarga yang mengalami gangguan jiwa akan membantu mempercepat dalam kesembuhan; Pengetahuan keluarga yang baik akan lebih baik dalam menghadapi anggota keluarga yang mengalami gangguan jiwa; Jenis kelamin keluarga yang mengantarkan ke rumah sakit jiwa cenderung laki-laki; Finansial, dimana keluarga yang memiliki finansial yang rendah akan mempengaruhi kepatuhan dalam pengobatan; Dan stigma dari masyarakat dimana seseorang yang mengalami gangguan jiwa akan di diskriminasi dan diabaikan di kelompok masyarakat.
Simpulan: Faktor-faktor yang mempengaruhi pemanfaatan pelayanan ke rumah sakit jiwa diantaranya yaitu aksesibilitas, sikap, pengetahuan yang dimiliki, jenis kelamin, dukungan finansial, serta stigma.
Keywords
References
Ali, S. H., & Agyapong, V. I. O. (2016). Barriers to Mental Health Service Utilisation in Sudan - Perspectives of Carers and Psychiatrists Health Systems and Services in Low and Middle Income Settings. BMC Health Services Research, 16(1). https://doi.org/10.1186/s12913-016-1280-2.
Alifariki, L. O. (2019). Analisis Faktor yang Berhubungan dengan Respon Keluarga Penderita Gangguan Jiwa Rawat Jalan di Rumah Sakit Jiwa Provinsi Sulawesi Tenggara. Faletehan Health Journal, 6(2), 69–74. www.journal.lppm-stikesfa.ac.id/ojs/index.php/FHJ.
Alluhaibi, B. A., & Awadalla, A. W. (2022). Attitudes and stigma toward seeking psychological help among Saudi Adults. BMC Psychology, 10(1). https://doi.org/10.1186/s40359-022-00923-4.
Buchman-Wildbaum, T., Váradi, E., Schmelowszky, Á., Griffiths, M. D., Demetrovics, Z., & Urbán, R. (2020). Targeting the Problem of Treatment Non-adherence Among Mentally Ill Patients: The Impact of Loss, Grief and Stigma. Psychiatry Research, 290. https://doi.org/10.1016/j.psychres.2020.113140.
Bruffaerts, R., Harris, M. G., Kazdin, A. E., Vigo, D. V., Sampson, N. A., Chiu, W. T., Al-Hamzawi, A., Alonso, J., Altwaijri, Y.A., Andrade, L., Benjet, C., & Kessler, R. C. (2022). Perceived helpfulness of treatment for social anxiety disorder: findings from the WHO World Mental Health Surveys. Social Psychiatry and Psychiatric Epidemiology, 57(10), 2079-2095.
Devi, H. N., Ahmed, N., & Roy, P. (2020). Attitude towards Treatment in Persons with Schizophrenia and Mood Disorders. Journal of Nursing and Health Science (IOSR-JNHS), 9(2), 40–45. https://www.iosrjournals.org/iosr-jnhs/papers/vol9-issue2/Series-2/E0902024045.pdf.
Devkota, G., Basnet, P., Thapa, B., & Subedi, M. (2021). Factors Affecting Utilization of Mental Health Services From Primary Health Care (PHC) Facilities of Western Hilly District of Nepal. PLoS ONE, 16(4 April). https://doi.org/10.1371/journal.pone.0250694.
Fettig, M., El-Hage, W., Klemina, I., Biberon, J., de Toffol, B., Thiriaux, A., Visseaux, J. F., Martin, M. L., Schwan, R., Bechiri, F., Cohn, A., Meyer, M., Maillard, L., & Hingray, C. (2020). Adherence to mental health care and caregiver-patient relationship after diagnosis of psychogenic non-epileptic seizures: Longitudinal follow-up study. Seizure, 80, 227–233. https://doi.org/10.1016/j.seizure.2020.06.001.
Fındık, O. T. P., Ceri, V., Ünver, H., Fiş, N. P., Arman, A. R., Beşer, C., Fadıloğlu, E., & Anagnostopoulos, D. (2021). Mental health need and psychiatric service utilization patterns of refugee children in Turkey: A comparative study. Children and youth services review, 124, 105970.
Gabra, R. H., Ebrahim, O. S., Osman, D. M. M., & Al-Attar, G. S. T. (2020). Knowledge, attitude and health-seeking behavior among family caregivers of mentally ill patients at Assiut University Hospitals: a cross-sectional study. Middle East Current Psychiatry, 27(1). https://doi.org/10.1186/s43045-020-0015-6
Idaiani, S., & Riyadi, E. I. (2018). Sistem Kesehatan Jiwa di Indonesia: Tantangan untuk Memenuhi Kebutuhan. Jurnal Penelitian Dan Pengembangan Pelayanan Kesehatan, 70–80. Diakses dari: https://doi.org/10.22435/jpppk.v2i2.134.
Kementerian Kesehatan Republik Indonesia. (2019). Situasi kesehatan jiwa di Indonesia. Jakarta: Pusat Data dan Informasi Kementerian Kesehatan RI (Infodatin).
Kementerian Kesehatan Republik Indonesia. (2022, October 11). Kemenkes Perkuat Jaringan Layanan Kesehatan Jiwa di Seluruh Fasyankes. Diakses dari: https://sehatnegeriku.kemkes.go.id/baca/umum/20221010/4041246/kemenkes-kembangkan-jejaring-pelayanan-kesehatan-jiwa-di-seluruh-fasyankes/.
Kusumawaty, I., Surahmat, R., Martini, S., & Mulyadi. (2021). Family Support For Members in Taking Care of Mental Disordered Patients. Atlantis Press.
Muhorakeye, O., & Biracyaza, E. (2021). Exploring Barriers to Mental Health Services Utilization at Kabutare District Hospital of Rwanda: Perspectives From Patients. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.638377.
Nabi, M., & Rizvi, T. (2022). Knowledge of Illness Among Family Caregivers of Psychiatric Patients. International Journal of Multidisciplinary Educational Research, 11(1). www.ijmer.in.
Olawande, T. I., Ajayi, M. P., Amoo, E. O., & Iruonagbe, C. T. (2019). Variations in Family Attitudes Towards Coping with People Living with Mental Illness. Open Access Macedonian Journal of Medical Sciences, 7(12), 2010–2016. https://doi.org/10.3889/oamjms.2019.071.
Poyraz Fındık, O. T., Fadıloğlu, E., Ay, P., & Fiş, N. P. (2022). Emergency mental health care for chi̇ldren and adolescents outside of regular working hours: 7 years outcomes from a tertiary hospital. Asian Journal of Psychiatry, 72. https://doi.org/10.1016/j.ajp.2022.103103.
Pradivta, R. D., Syafrini, R. O., & Mulyani, S. (2020). Hubungan Pelaksanaan Tugas Keluarga Dengan Penerimaan Keluarga Terhadap Pasien Skizofrenia. Jurnal Ilmiah Ners Indonesia, 1(2).
Primananda, A. P. (2022, August 16). Definisi Mental Illness (Gangguan Mental). Direktorat Jenderal Pelayanan Kesehatan. Diakses dari: https://yankes.kemkes.go.id/view_artikel/1314/definisi-mental-illnessgangguan-mental.
Rahman, S., & Permana, I. (2020). Penerimaan Keluarga Dalam Perawatan Orang Dengan Skizofrenia Di Masyarakat Banjar Kalimantan Selatan. Dinamika Kesehatan Jurnal Kebidanan Dan Keperawatan , 10(1), 380–387. https://doi.org/10.33859/dksm.v10i1.424.
Seid, A., Wordofa, B., & Tesfaye, J. (2021). Utilization of Modern Family Planning Method Among Women With Psychiatric Disorders at Amanuel Mental Health Specialized Hospital Addis Ababa, Ethiopia, 2018. Ethiopian Journal of Reproductive Health, 13(1).
Tirintica, A. R., Andjelkovic, I., Sota, O., Pirlog, M. C., Stoyanova, M., Mihai, A., & Wallace, N. (2018). Factors That Influence Access to Mental Health Services in South-Eastern Europe. International Journal of Mental Health Systems, 12(1). https://doi.org/10.1186/s13033-018-0255-6.
Tristiana, R. D., Triantoro, B., Nihayati, H. E., Yusuf, A., & Abdullah, K. L. (2019). Relationship Between Caregivers’ Burden of Schizophrenia Patient with Their Quality of Life in Indonesia. Journal of Psychosocial Rehabilitation and Mental Health, 6(2), 141–148. https://doi.org/10.1007/s40737-019-00144-w.
Vázquez, A. L., de la Caridad Alvarez, M., Flores, C. M. N., Vera, J. M. G., Barrett, T. S., & Rodríguez, M. M. D. (2021). Youth mental health service preferences and utilization patterns among Latinx caregivers. Children and Youth Services Review, 131, 106258. https://doi.org/10.1016/j.childyouth.2021.106258.
Victor, C. K., Gilbert, M. M., Ondora, O. M., & Abel, K. O. (2022). Barriers to Mental Health Services Utilization Among Outpatient Clinic Attendees at Mathari National Teaching and Referral hospital, Nairobi City, Kenya. International Journal Of Community Medicine And Public Health, 9(6), 2431. https://doi.org/10.18203/2394-6040.ijcmph20221516
World Health Organization. (2022, June 8). Mental disorders. Diakses dari: https://www.who.int/news-room/fact-sheets/detail/mental-disorders.
Xanthopoulou, P. D., Mbanu, J., Chevalier, A., Webber, M., & Giacco, D. (2022). Social Isolation and Psychosis: Perspectives from People with Psychosis, Family Caregivers and Mental Health Professionals. Community mental health journal, 58(7), 1338-1345.
Yusuf, A. (2020, July 9). Telaah Sistematik Penerimaan Keluarga Terhadap Pasien Skizofrenia. UNAIR News. https://news.unair.ac.id/2020/07/09/telaah-sistematik-penerimaan-keluarga-terhadap-pasien-skizofrenia/.
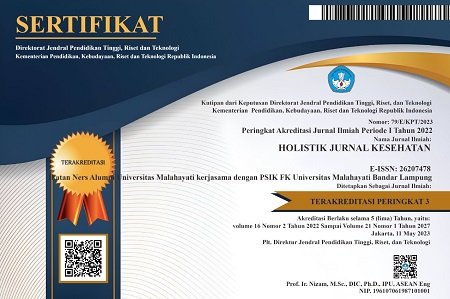
DOI: https://doi.org/10.33024/hjk.v17i2.9338
Refbacks
- There are currently no refbacks.
Copyright (c) 2023 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.