Penerapan Introduction, Situation, Background, Assessment and Recommendation (ISBAR) untuk komunikasi efektif antara perawat dan dokter di Rumah Sakit Umum Daerah Cibabat Kota Cimahi
Abstract
ISBAR and effective communication between nurses and doctors
Background: The communication errors the main cause of events reported to the United States Joint Commission between 1995 to 2006 of 25000-30000 preventable incidents that cause permanent disability. 11% of these adverse events are due to 6% different communication problems and also because inadequate level of skills. In Indonesia, data on unexpected-events (UEs)) let alone the event of near‐miss events (NMEs) is still scarce, but on the other hand there is an increase in accusations of "mal practice", which is not necessarily in accordance with the final proof, Patient safety targets, the main element of care services to patients is effective communication. At Cibabat hospital uses SBAR communication between nurses and doctors, but there is still an element lacking in the nurse's self-introduction component when calling doctors
Purpose: This study aims to determine the description and effectiveness of ISBAR communication as effective communication between nurses and doctors
Methods: The sample of 79 nurses by survey and another nurses of 45 by observation, it done in ICU and inpatient ward. Surveys Questioners filled up direct by respondents and observation sheets filled up by supervisors through look directly at the moment a communication. The data collected is analyzed by frequency distribution from the results of surveys and all data analized by a statistical test to find the effectiveness of communication with the Wilcoxon Test
Results: The survey found that has improved of 80% to 93.3% (ICU) and of 78.1% to 87.5% (Inpatient ward) of the communication component Introduction; by mention the name. Observation results introduction; mention the name of ISBAR communication there was a significant improve from 57.1% to 100% (ICU) and from 20.8% to 79.2% (inpatient ward). Wilcoxon test results were found from observations in ICU with a value of 0.003 (p <0.05) and in the inpatient ward with a value of 0.00 (p <0.05) for the introduction aspect. Therefore, this study found that ISBAR communication more effective than SBAR in terms of mentioning the names in the aspects of Introduction
Conclusion: That ISBAR Communication is more effective than SBAR communication in terms of the component of name's Introduction aspect. As a result, ISBAR communication can be implemented as a standard of communication for Cibabat General Hospital and other hospitals.
Keywords: ISBAR; Communication; Effective; Nurses and Doctors; Hospital
Pendahuluan: Kesalahan dalam komunikasi adalah penyebab utama peristiwa yang dilaporkan ke Komisi Bersama Amerika Serikat antara 1995 dan 2006 yaitu dari 25000-30000 kejadian buruk yang dapat dicegah menyebabkan cacat permanen 11% kejadian buruk ini adalah karena masalah komunikasi yang berbeda 6% dan juga karena tidak memadai tingkat ketrampilannya. Di Indonesia data tentang kejadian tidak diharapkan (KTD) apalagi kejadian nyaris cedera (KNC) masih langka, namun di lain pihak terjadi peningkatan tuduhan “mal praktek”, yang belum tentu sesuai dengan pembuktian akhir. Sasaran keselamatan pasien, unsur yang utama dari layanan asuhan ke pasien adalah komunikasi efektif.RSUD Cibabat menggunakan komunikasi SBAR dalam komunikasi dengan dokter, tapi masih ada unsur kurang dalam komponen mengenalakan diri perawat saat menelpon dokter
Tujuan: Penelitian ini bertujuan untuk mengetahui gambaran dan keefectivan komunikasi ISBAR sebagai komunikasi efektif antara perawat dan dokter
Metode: Penelitian ini menggunakan sampel sebanyak 79 perawat untuk survey ruang ICU dan rawat inap dan 45 perawat untuk observasi di ruang ICU dan rawat inap. Questioner di berikan kepada responden survey dan lembar observasi di berikan kepada tim Supervisor rumah sakit dengan melihat langsung komunikasi yang dilakukan. Data yang terkumpul di analisa dengan disribusi frequency dari hasil survey dan observasi dan kemudian data observasi di lakukan uji statsistik untuk melihat keefectivan dengan Uji Wilcoxon
Hasil: Hasil penelitian didapatkan untuk Survey ditemukan bahwa peningkatan dari dari 80% menjadi 93,3%. (ICU) dan 78,1 % menjadi 87,5% (Rawat inap) dari komponen komunikasi Introduction; menyebutkan nama. Hasil observasi Introduction; menyebutkan nama dari komunikasi ISBAR terjadi peningkatan significan dari 57,1 % menjadi 100% (ICU) dan dari 20,8% menjadi 79,2 % (Rawat inap). Uji hasil test wilcoxon ditemukan dari hasil observasi di ruang ICU dengan nilai 0,003 (p< 0.05) dan di ruang rawat inap dengan nilai 0,00 (p< 0,05) untuk aspek introduction. Sehingga dari penelitian ini disimpulkan bahwa Komunikasi ISBAR lebih efective untuk diterapkan dari pada komunikasi SBAR dalam hal komponen Meneyebutkan nama di aspek Introduction
Simpulan: penelitian ini menyimpulkan bahwa Komunikasi ISBAR lebih efective untuk diterapkan dari pada komunikasi SBAR dalam hal komponen menyebutkan nama di aspek Introduction. Sehingga komunikasi ISBAR bisa jadikan standard komunikasi untuk RSUD Cibabat Khususnya dan Rumah sakit lain pada umumnya.
Keywords
Full Text:
PDFReferences
Abdellatif, A., Bagian, J. P., Barajas, E. R., Cohen, M., Cousins, D., Denham, C. R, & Horvath, D. (2007). Communication During Patient Hand-Overs: Patient Safety Solutions, Volume 1, Solution 3, May 2007. Joint Commission Journal on Quality and Patient Safety, 33(7), 439-442.
Aldrich, R., Duggan, A., Lane, K., Nair, K., & Hill, K. (2009). ISBAR revisited: identifying and solving barriers to effective clinical handover in inter-hospital transfer–public report on pilot study. Newcastle: Hunter New England Health
Bost, N., Crilly, J., Patterson, E., & Chaboyer, W. (2012). Clinical handover of patients arriving by ambulance to a hospital emergency department: a qualitative study. International Emergency Nursing, 20(3), 133-141
Departemen Kesehatan Republik Indonesia. (2008). Panduan nasional keselamatan pasien rumah sakit (patient safety). Edited by, 2.
Dewi, M. (2012). Pengaruh pelatihan timbang terima pasien terhadap penerapan keselamatan pasien oleh perawat pelaksana di RSUD Raden Mattaher Jambi. Jurnal Health and Sport, 5(03).
Fealy, G., Munroe, D., Riordan, F., Croke, E., Conroy, C., McNamara, M., & Shannon, M. (2016). Clinical handover practices in maternity services in Ireland: A qualitative descriptive study. Midwifery, 39, 20-26
Foronda, C., MacWilliams, B., & McArthur, E. (2016). Interprofessional communication in healthcare: An integrative review. Nurse education in practice, 19, 36-40
Kitney, P., Tam, R., Bennett, P., Buttigieg, D., Bramley, D., & Wang, W. (2016). Handover between anaesthetists and post-anaesthetic care unit nursing staff using ISBAR principles: A quality improvement study. ACORN: The Journal of Perioperative Nursing in Australia, 29(1), 30.
Mullany, D. V., Ziegenfuss, M., Goleby, M. A., & Ward, H. E. (2016). Improved hospital mortality with a low MET dose: the importance of a modified early warning score and communication tool. Anaesthesia and intensive care, 44(6), 734-741
Pang, W. I. (2017). Promoting integrity of shift report by applying ISBAR principles among nursing students in clinical placement. In SHS Web of Conferences (Vol. 37, p. 01019). EDP Sciences.
Pascoe, H., Gill, S. D., Hughes, A., & McCall-White, M. (2014). Clinical handover: An audit from Australia. The Australasian medical journal, 7(9), 363.
Ramasubbu, B., Stewart, E., & Spiritoso, R. (2017). Introduction of the identification, situation, background, assessment, recommendations tool to improve the quality of information transfer during medical handover in intensive care. Journal of the intensive care society, 18(1), 17-23
Solutions, P. S. (2007). Communication during patient hand-overs. World Health Organization
Spooner, A. J., Aitken, L. M., Corley, A., Fraser, J. F., & Chaboyer, W. (2016). Nursing team leader handover in the intensive care unit contains diverse and inconsistent content: An observational study. International journal of nursing studies, 61, 165-172.
Triwibowo, C., Yuliawati, S., & Husna, N. A. (2018). Handover Sebagai upaya Peningkatan Keselamatan Pasien (Patient Safety) di Rumah Sakit. Jurnal Keperawatan Soedirman, 11(2), 76-80.
Wainwright, C., & Wright, K. M. (2016). Nursing clinical handover improvement practices among acute inpatients in a tertiary hospital in Sydney: a best practice implementation project. JBI database of systematic reviews and implementation reports, 14(10), 263-275.
World Health Organization. (2007). Communication during patient hand-overs. Patient safety solutions, 1(3), 1-4.
World Health Organization. (2008). World alliance for patient safety: forward programme 2008-2009 (No. WHO/IER/PSP/2008.04). Geneva: World Health Organization
Yulia, S. (2010). Pengaruh pelatihan keselamatan pasien terhadap pemahaman perawat pelaksana mengenai penerapan keselamatan pasien di RS Tugu Ibu Depok
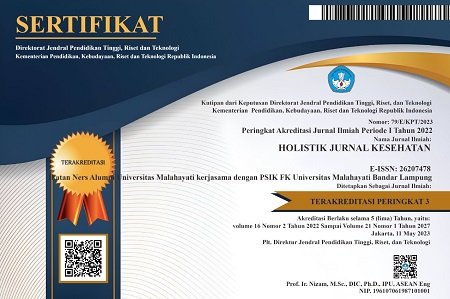
DOI: https://doi.org/10.33024/hjk.v13i4.1587
Refbacks
Copyright (c) 2019 HOLISTIK JURNAL KESEHATAN

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.