Pencegahan Kejadian Ventilator-Associated Pneumonia (VAP) dengan Kepatuhan Pelaksanaan Bundle: Literature Review
Abstract
Prevention of Ventilator-Associated Pneumonia (VAP) Events with Compliance with Bundle Implementation: Literature Review
Background: Patients who experience critical illness and use a mechanical ventilator in the ICU have an increased risk of experiencing ventilator associated pneumonia (VAP) which is a major cause of morbidity and mortality in the ICU and causes lengthening the length of stay and an increase in hospital costs.
Purpose: To conduct a recent literature review with regard to VAP primarily related to causes, risk factors, pathogenesis, prevention, early detection and diagnosis, and administration of antibiotics to patients with VAP. At the end of this article conclusions will be presented that can be used by practitioners as a clinical guide.
Method: The design used was literature review, articles were collected using a search engine, including (Clinicalkey) 27 articles, (Cochrane) 25 articles, (Medline) 17 articles and (Pubmed) 19 articles. From the predetermined article inclusion criteria, we found 7 articles out of 88 that were suitable for different interventions
Results: Prevention of VAP incidents in hospitals using multimodal interventions, one of which is the application of a VAP prevention bundle, can effectively reduce the incidence of VAP in hospitals. Examination of the lower respiratory tract culture should be carried out for all patients before administering antibiotic therapy provided that it should not delay giving antibiotic therapy to critical patients. Early treatment of broad-spectrum antibiotics with the right dosage can maximize the efficacy of antibiotics and the outcome of VAP patients in the ICU. Antibiotic combinations must be used wisely to treat VAP because certain pathogens increase the life expectancy of patients with severe infections especially those with septic shock. Negative culture results can also be used to stop antibiotic therapy in patients undergoing culture without antibiotic changes within the last 72 hours. The health team must consider the need for antibiotic de-escalation based on the culture results and the clinical response of the patient.
Conclusion: VAP prevention bundles that implement multimodal interventions effectively reduce the incidence of VAP in hospitals. An examination of airway culture must be carried out for all patients before administering antibiotic therapy. Early treatment of broad-spectrum antibiotics can maximize the efficacy of antibiotics and the outcome of VAP patients in the ICU.
Keywords: VAP; ICU; Patients; Morbidity; Mortality; Bundle
Pendahuluan: Pasien yang mengalami penyakit kritis dan menggunakan ventilator mekanik di ICU mempunyai peningkatan resiko untuk mengalami ventilator associated pneumonia (VAP) yang merupakan penyebab utama morbiditas dan mortalitas di ICU serta menyebabkan pemanjangan lenght of stay dan peningkatan biaya rumah sakit.
Tujuan: Untuk melakukan review literature terkini sehubungan dengan VAP terutama terkait dengan penyebab, faktor resiko, pathogenesis, pencegahan, deteksi dini dan diagnosis, serta pemberian antibiotik pada pasien dengan VAP. Di ahir artikel ini akan disampaikan kesimpulan yang dapat digunakan praktisi sebagai panduan di klinis.
Metode: Desain yang digunakan adalah literature review, artikel dikumpulkan menggunakan mesin pencarian antara lain (Clinicalkey) 27 artikel, (Cochrane) 25 artikel, (Medline) 17 artikel dan (Pubmed) 19 artikel. Dari kriteria inklusi artikel yang telah ditentukan, ditemukan 7 artikel dari 88 yang sesuai dengan intervensi yang berbeda.
Hasil: Pencegahan kejadian VAP di rumah sakit menggunakan intervensi multimodal, yang mana salah satunya berupa penerapan bundle pencegahan VAP, dapat dengan efektif menurunkan kejadian VAP di rumah sakit. Pemeriksasan kultur saluran nafas bawah perlu dilakukan kepada semua pasien sebelum pemberian terapi antibiotik dengan catatan tidak boleh menunda pemberian terapi antibiotik pada pasien kritis. Terapi dini antibiotik spektum luas dengan dosis yang tepat dapat memaksimalkan kemanjuran antibiotik dan luaran pasien VAP di ICU. Kombinasi antibiotik harus digunakan dengan bijaksana untuk mengobati VAP karena pathogen tertentu untuk meningkatkan harapan hidup pasien dengan infeksi berat terutama yang mengalami shok sepsis. Hasil kultur yang negatif juga dapat digunakan untuk menghentikan terapi antibiotik pada pasien yang dilakukan kultur tanpa perubahan antibiotik dalam 72 jam terahir. Tim kesehatan harus mempertimbangkan perlunya deeskalasi antibiotik berdasarkan hasil kultur dan respon klinik pasien.
Simpulan: Bundle pencegahan VAP yang menerapkan intervensi multimodal efektif menurunkan kejadian VAP di rumah sakit. Pemeriksasan kultur saluran nafas harus dilakukan kepada semua pasien sebelum pemberian terapi antibiotik. Terapi dini antibiotik spektum luas dapat memaksimalkan kemanjuran antibiotik dan luaran pasien VAP di ICU.
Keywords
References
Akdogan, O., Ersoy, Y., Kuzucu, C., Gedik, E., Togal, T., & Yetkin, F. (2017). Assessment of the effectiveness of a ventilator associated pneumonia prevention bundle that contains endotracheal tube with subglottic drainage and cuff pressure monitorization. The Brazilian Journal of Infectious Diseases, 21(3), 276–281. https://doi.org/10.1016/j.bjid.2017.01.002
Alp, E., & Voss, A. (2006). Ventilator associated pneumonia and infection control. Annals of Clinical Microbiology and Antimicrobials, 5, 7. https://doi.org/10.1186/1476-0711-5-7
Arthur, L. E., Kizor, R. S., Selim, A. G., van Driel, M. L., & Seoane, L. (2016). Antibiotics for ventilator-associated pneumonia. The Cochrane Database of Systematic Reviews, 10, CD004267. https://doi.org/10.1002/14651858.CD004267.pub4
Berry, A. M., Davidson, P. M., Nicholson, L., Pasqualotto, C., & Rolls, K. (2011). Consensus based clinical guideline for oral hygiene in the critically ill. Intensive and Critical Care Nursing, 27(4), 180–185. https://doi.org/10.1016/j.iccn.2011.04.005
Djordjevic, Z. M., Folic, M. M., & Jankovic, S. M. (2017). Distribution and antibiotic susceptibility of pathogens isolated from adults with hospital-acquired and ventilator-associated pneumonia in intensive care unit. Journal of Infection and Public Health, 10(6), 740–744. https://doi.org/10.1016/j.jiph.2016.11.016
Dodek, P., Keenan, S., Cook, D., Heyland, D., Jacka, M., Hand, L., Muscedere, J., Foster, D., Mehta, N., Hall, R., Brun-Buisson, C., & for the Canadian Critical Care Trials Group and the Canadian Critical Care Society. (2004). Evidence-Based Clinical Practice Guideline for the Prevention of Ventilator-Associated Pneumonia. Annals of Internal Medicine, 141(4), 305. https://doi.org/10.7326/0003-4819-141-4-200408170-00011
Gunasekera, P., & Gratrix, A. (2016). Ventilator-associated pneumonia. BJA Education, 16(6), 198–202. https://doi.org/10.1093/bjaed/mkv046
Hua, F., Xie, H., Worthington, H. V., Furness, S., Zhang, Q., & Li, C. (2016). Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD008367.pub3
Jaimes, F., De La Rosa, G., Gómez, E., Múnera, P., Ramírez, J., & Castrillón, S. (2007). Incidence and risk factors for ventilator-associated pneumonia in a developing country: Where is the difference? Respiratory Medicine, 101(4), 762–767. https://doi.org/10.1016/j.rmed.2006.08.008
Kalanuria, A. A., Zai, W., & Mirski, M. (2014). Ventilator-associated pneumonia in the ICU. Critical Care, 8.
Kao, C.-C., Chiang, H.-T., Chen, C.-Y., Hung, C.-T., Chen, Y.-C., Su, L.-H., Shi, Z.-Y., Liu, J.-W., Liu, C.-P., Chuang, Y.-C., Ko, W.-C., Chen, Y.-H., Tseng, S.-H., Lee, C.-M., Lu, M.-C., & Hsueh, P.-R. (2019). National bundle care program implementation to reduce ventilator-associated pneumonia in intensive care units in Taiwan. Journal of Microbiology, Immunology and Infection, 52(4), 592–597. https://doi.org/10.1016/j.jmii.2017.11.001
Kumar, A., Safdar, N., Kethireddy, S., & Chateau, D. (2010). A survival benefit of combination antibiotic therapy for serious infections associated with sepsis and septic shock is contingent only on the risk of death: A meta-analytic/meta-regression study. Critical Care Medicine, 38(8), 1651–1664. https://doi.org/10.1097/CCM.0b013e3181e96b91
Lee, P.-L., Lee, W.-T., & Chen, H.-L. (2017). Ventilator-Associated Pneumonia in Low Birth Weight Neonates at a Neonatal Intensive Care Unit: A Retrospective Observational Study. Pediatrics & Neonatology, 58(1), 16–21. https://doi.org/10.1016/j.pedneo.2015.10.014
Leone, M., Bouadma, L., Bouhemad, B., Brissaud, O., Dauger, S., Gibot, S., Hraiech, S., Jung, B., Kipnis, E., Launey, Y., Luyt, C.-E., Margetis, D., Michel, F., Mokart, D., Montravers, P., Monsel, A., Nseir, S., Pugin, J., Roquilly, A., … Chanques, G. (2018). Hospital-acquired pneumonia in ICU. Anaesthesia Critical Care & Pain Medicine, 37(1), 83–98. https://doi.org/10.1016/j.accpm.2017.11.006
Ma, S., Liu, S., Huang, L., Xu, C., Liu, W., & Huang, Y. (2014). A meta analysis of the effect of enhanced hand hygiene on the morbidity of ventilator-associated pneumonia. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue, 26(5), 304–308. https://doi.org/10.3760/cma.j.issn.2095-4352.2014.05.004
Miller, D. F. (2018). Ventilator-Associated Pneumonia. Intensive Care, 6.
Nseir, S., Lorente, L., Ferrer, M., Rouzé, A., Gonzalez, O., Bassi, G. L., Duhamel, A., & Torres, A. (2015). Continuous control of tracheal cuff pressure for VAP prevention: A collaborative meta-analysis of individual participant data. Annals of Intensive Care, 5. https://doi.org/10.1186/s13613-015-0087-3
Özçaka, Ö., Başoğlu, O. K., Buduneli, N., Taşbakan, M. S., Bacakoğlu, F., & Kinane, D. F. (2012). Chlorhexidine decreases the risk of ventilator-associated pneumonia in intensive care unit patients: A randomized clinical trial. Journal of Periodontal Research, 47(5), 584–592. https://doi.org/10.1111/j.1600-0765.2012.01470.x
Sebastian, M., Lodha, R., Kapil, A., & Kabra, S. (2012). Oral mucosal decontamination with chlorhexidine for the prevention of ventilator-associated pneumonia in children—A randomized, controlled trial. Pediatric Critical Care Medicine, 13(5), 305–310.
Silva, A. R. A. da, Silva, T. C. da, Bom, G. J. T., Vasconcelos, R. M. B., & Junior, R. S. (2018). Ventilator-associated pneumonia agents in Brazilian Neonatal Intensive Care Units – a systematic review. The Brazilian Journal of Infectious Diseases, 22(4), 338–344. https://doi.org/10.1016/j.bjid.2018.06.002
Strategy for the Control of Antimicrobial Resistance in Ireland, & Health Protection Surveillance Centre (Ireland). (2011). Guidelines for the prevention of ventilator-associated pneumonia in adults in Ireland. Health Protection Surveillance Centre.
Tablan, O., Anderson, L., Besser, R., Bridges, C., & Hajjeh, R. (2004). Guidelines for Preventing Health-Care-Associated Pneumonia, 2003: Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (pp. 1–179) [Data set]. American Psychological Association. https://doi.org/10.1037/e548652006-001
The American Thoracic Society, & The Infectious Diseases Society of America. (2005). Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. American Journal of Respiratory and Critical Care Medicine, 171(4), 388–416. https://doi.org/10.1164/rccm.200405-644ST
Wang, C.-H., Ho, Y.-H., Jiang, H.-L., Wang, L.-S., Cheng, L.-C., Ho, G.-J., Chung, H.-C., Huang, X.-H., & Xu, Y.-P. (2015). Efficacy of ventilator-associated pneumonia bundle in the surgical intensive care unit. Journal of Microbiology, Immunology and Infection, 48(2), S162. https://doi.org/10.1016/j.jmii.2015.02.565
Wang, L., Li, X., Yang, Z., Tang, X., Yuan, Q., Deng, L., & Sun, X. (2016). Head bed elevation versus flat bed for preventing ventilator-associated pneumonia (VAP) in adults requiring mechanical ventilation. Cochrane. https://doi.org/10.1002/14651858.CD009946.pub2
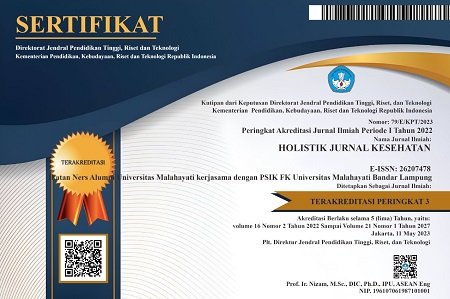
DOI: https://doi.org/10.33024/hjk.v14i3.2661
Refbacks
- There are currently no refbacks.
Copyright (c) 2020 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.