Studi literatur: Efektivitas weaning ventilasi mekanik dengan pressure support ventilation (PSV) vs T-piece
Abstract
The effectiveness of mechanical ventilation weaning with pressure support ventilation (PSV) vs T-piece: A Literature study
Background: Prolonged mechanical ventilation can increase the risk of infection, length of stay in the ICU, length of hospital stay, mortality, and cost of healthcare. The mechanical ventilation weaning process can be done using the pressure support (PSV) method or using a T-Piece.
Purpose: Determine the effectiveness of the PSV vs T-Piece method in mechanical ventilation weaning.
Method: The literature research uses electronic databases including PubMed, CINAHL, Proquest, and google scholar. Keywords for data search are using the keywords "SBT", "Pressure support", "T-piece", "weaning mechanical ventilation". Inclusion criteria: English-language journal, RCT design, published from 2010 to 2020, and full text.
Results: The results were five RCT studies with a total number of respondents as many as 2038 patients. Two studies suggest that both the PSV and the T-piece methods have the same success rate. Three studies stated that there was no difference in the reintubation rate <48 hours, the mortality rate, and the length of the stay in the hospital. The length of stay in the ICU from five studies also suggested no difference.
Conclusion: The mechanical ventilation weaning method or SBT with the PSV and T-Piece methods in general there is no difference in the success rate or in the outcomes.
Keywords: Weaning Mechanical Ventilation; Effectiveness; PSV T-Piece
Pendahuluan: Prolong ventilasi mekanik dapat meningkatkan resiko infeksi, lama rawat ICU, lama rawat rumah sakit dan mortalitas serta biaya perawatan. Proses weaning ventilasi mekanik dapat dilakukan dengan metode pressure support (PSV) atau menggunakan T-Piece.
Tujuan: Mengetahui efektivitas metode PSV vs T-Piece dalam weaning ventilasi mekanik.
Metode: Pencarian literature menggunakan database elektronik termasuk didalamnya PubMed, CINAHL, Proquest dan google scholar. Kata kunci pencarian data yaitu dengan menggunakan kata kunci “SBT”, “Pressure support”, “T-piece”, “weaning mechanical ventilation”. kriteri inklusi: jurnal berbahasa inggris, desain RCT, dipublikasikan dari tahun 2010 sampai dengan 2020, dan full text.
Hasil: Ada lima Studi RCT dengan Total jumlah reponden sebanyak 2038 pasien. Dua studi menyatakan bahwa baik metode PSV dan T-piece mempunyai tingkat keberhasilan yang sama. Dari tiga studi menyatakan bahwa angka kejadian reintubasi < 48 jam tidak ada perbedaan, angka mortalitas dan lama rawat ICU dari lima studi tidak ada perbedaan. Dari tiga studi lama rawat di rumah sakit tidak ada perbedaan.
Simpulan: Metode weaning ventilasi mekanik atau SBT dengan metode PSV dan T-Piece secara umum tidak ada perbedaan dalam tingkat keberhasilan maupun dalam outcomenya.
Keywords
References
Azoulay, E., Pène, F., Darmon, M., Lengliné, E., Benoit, D., Soares, M., & en Réanimation, G. D. R. R. (2015). Managing critically ill hematology patients: time to think differently. Blood reviews, 29(6), 359-367.
Camporota, L., & Barrett, N. (2016). Current applications for the use of extracorporeal carbon dioxide removal in critically ill patients. BioMed research international, 2016.
Chittawatanarat, K., Orrapin, S., Jitkaroon, K., Mueakwan, S., & Sroison, U. (2018). An Open Label Randomized Controlled Trial to Compare Low Level Pressure Support and T-piece as Strategies for Discontinuation of Mechanical Ventilation in a General Surgical Intensive Care Unit. Medical Archives (Sarajevo, Bosnia and Herzegovina), 72(1), 51–57. https://doi.org/10.5455/medarh.2018.72.51-57
De Jong, A., Calvet, L., Lemiale, V., Demoule, A., Mokart, D., Darmon, M., & Azoulay, E. (2018). The challenge of avoiding intubation in immunocompromised patients with acute respiratory failure. Expert review of respiratory medicine, 12(10), 867-880.
Diaconu, O., Siriopol, I., Poloșanu, L. I., & Grigoraș, I. (2018). Endotracheal tube biofilm and its impact on the pathogenesis of ventilator-associated pneumonia. The Journal of Critical Care Medicine, 4(2), 50.
Ebrahimabadi, S., Moghadam, A. B., Vakili, M., Modanloo, M., & Khoddam, H. (2017). Studying the power of the integrative weaning index in predicting the success rate of the spontaneous breathing trial in patients under mechanical ventilation. Indian Journal of Critical Care Medicine, 21(8), 488–493. https://doi.org/10.4103/ijccm.IJCCM_10_17
Fang, T. P., Chen, Y. J., Yang, T. M., Wang, S. H., Hung, M. S., Chiu, S. H., & Lin, H. L. (2020). Optimal connection for Tiotropium SMI delivery through mechanical ventilation: an in vitro study. Pharmaceutics, 12(3), 291.
Fernandez, M. M., González-Castro, A., Magret, M., Bouza, M. T., Ibañez, M., García, C., Balerdi, B., Mas, A., Arauzo, V., Añón, J. M., Ruiz, F., Ferreres, J., Tomás, R., Alabert, M., Tizón, A. I., Altaba, S., Llamas, N., & Fernandez, R. (2017). Reconnection to mechanical ventilation for 1 h after a successful spontaneous breathing trial reduces reintubation in critically ill patients: a multicenter randomized controlled trial. Intensive Care Medicine, 43(11), 1660–1667. https://doi.org/10.1007/s00134-017-4911-0
Kotfis, K., Wittebole, X., Jaschinski, U., Solé-Violán, J., Kashyap, R., Leone, M., ... & ICON Investigators. (2019). A worldwide perspective of sepsis epidemiology and survival according to age: Observational data from the ICON audit. Journal of critical care, 51, 122-132.
Loss, S. H., De Oliveira, R. P., Maccari, J. G., Savi, A., Boniatti, M. M., Hetzel, M. P., Dallegrave, D. M., De Campos Balzano, P., Oliveira, E. S., Höher, J. A., Torelly, A. P., & Teixeira, C. (2015). The reality of patients requiring prolonged mechanical ventilation: A multicenter study. Revista Brasileira de Terapia Intensiva, 27(1), 26–35.
Lourenço, I. S., Franco, A. M., Bassetto, S., & Rodrigues, A. J. (2013). Pressure support-ventilation versus spontaneous breathing with" T-Tube" for interrupting the ventilation after cardiac operations. Brazilian Journal of Cardiovascular Surgery, 28, 455-461. https://doi.org/10.5935/1678-9741.20130075
Maggiore, S. M., Battilana, M., Serano, L., & Petrini, F. (2018). Ventilatory support after extubation in critically ill patients. The Lancet Respiratory Medicine, 6(12), 948-962.
Pellegrini, J. A. S., Boniatti, M. M., Boniatti, V. C., Zigiotto, C., Viana, M. V., Nedel, W. L., da Silva Marques, L., dos Santos, M. C., de Almeida, C. B., Dal’ Pizzol, C. P., Ziegelmann, P. K., & Vieira, S. R. R. (2018). Pressure-support ventilation or T-piece spontaneous breathing trials for patients with chronic obstructive pulmonary disease - A randomized controlled trial. PLoS ONE, 13(8), 1–15. https://doi.org/10.1371/journal.pone.0202404
Pellegrini, J. A. S., Moraes, R. B., Maccari, J. G., de Oliveira, R. P., Savi, A., Ribeiro, R. A., Burns, K. E. A., & Teixeira, C. (2016). Spontaneous breathing trials with T-piece or pressure support ventilation. Respiratory Care, 61(12), 1693–1703. https://doi.org/10.4187/respcare.04816
Rabinstein, A. A. (2015). Acute neuromuscular respiratory failure. CONTINUUM: Lifelong Learning in Neurology, 21(5), 1324-1345.
Raoof, S., Nava, S., Carpati, C., & Hill, N. S. (2020). How I Do It: High Flow, Non-invasive ventilation and Awake (non-intubation) Proning in Covid-19 Patients with Respiratory Failure. Chest.
Resende, M. M., Monteiro, S. G., Callegari, B., Figueiredo, P. M. S., Monteiro, C. R. A. V., & Monteiro-Neto, V. (2013). Epidemiology and outcomes of ventilator-associated pneumonia in northern Brazil: An analytical descriptive prospective cohort study. BMC Infectious Diseases, 13(1). https://doi.org/10.1186/1471-2334-13-119
Santos Pellegrini, J. A., Boniatti, M. M., Boniatti, V. C., Zigiotto, C., Viana, M. V., Nedel, W. L., & Rios Vieira, S. R. (2018). Pressure-support ventilation or T-piece spontaneous breathing trials for patients with chronic obstructive pulmonary disease-A randomized controlled trial. PloS one, 13(8), e0202404.
Sklar, M. C., Dres, M., Fan, E., Rubenfeld, G. D., Scales, D. C., Herridge, M. S., & Goligher, E. C. (2020). Association of low baseline diaphragm muscle mass with prolonged mechanical ventilation and mortality among critically ill adults. JAMA network open, 3(2), e1921520-e1921520.
Subirà, C., Hernández, G., Vázquez, A., Rodríguez-Garciá, R., González-Castro, A., Garciá, C., Rubio, O., Ventura, L., López, A., De La Torre, M. C., Keough, E., Arauzo, V., Hermosa, C., Sánchez, C., Tizón, A., Tenza, E., Laborda, C., Cabañes, S., Lacueva, V., & Fernández, R. (2019). Effect of pressure support vs T-piece ventilation strategies during spontaneous breathing trials on successful extubation among patients receiving mechanical ventilation: A randomized clinical trial. JAMA - Journal of the American Medical Association, 321(22), 2175–2182. https://doi.org/10.1001/jama.2019.7234
Teixeira, S. N., Osaku, E. F., de Macedo Costa, C. R. L., Toccolini, B. F., Costa, N. L., Cândia, M. F., Leite, M. A., Jorge, A. C., & Duarte, P. A. D. (2015). Comparison of proportional assist ventilation plus, T-tube ventilation, and pressure support ventilation as spontaneous breathing trials for extubation: A randomized study. Respiratory Care, 60(11), 1527–1535. https://doi.org/10.4187/respcare.03915
Torres, A., Niederman, M. S., Chastre, J., Ewig, S., Fernandez-Vandellos, P., Hanberger, H., & Wunderink, R. (2017). International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociación Latinoamericana del Tórax (ALAT). European Respiratory Journal, 50(3).
DOI: https://doi.org/10.33024/hjk.v15i3.4295
Refbacks
- There are currently no refbacks.
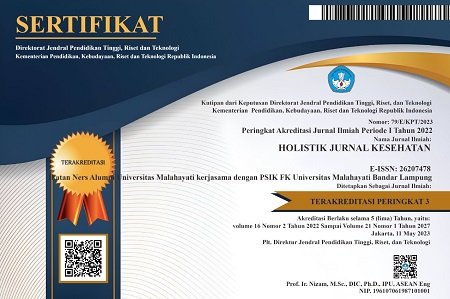
Copyright (c) 2021 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.