Implementasi layanan telemedicine di masa pandemi Covid-19: Literature review
Abstract
Background: Telemedicine is a remote health service using audio, visual, and data communications, including treatment, diagnosis, consultation, and treatment, as well as the exchange of medical data. In the implementation of telemedicine services, cooperation from various parties is needed, including patients and health care facilities.
Purpose: To analyze the implementation of telemedicine services during the Covid-19 pandemic.
Method: A literature review study with the PubMed, ScienceDirect, and Google Scholar databases. The assessment and quality of articles in this research use the Preferred Reporting Items for Systematic Review and Meta-Analysis instrument.
Results: Based on the search results, obtained 9 articles that are relevant and in accordance with the research inclusion criteria. From these 9 articles, got 5 related to implementing telemedicine services and 3 factors that can affect telemedicine services..
Conclusion: 5 matters related to implementing telemedicine namely the advantages and disadvantages, benefits, influencing factors, and implementation of telemedicine services during the Covid-19 pandemic. In addition, 3 factors can affect telemedicine services, namely finance, technology infrastructure, and organizational rules and regulations.
Keywords: Covid-19; Implementation; Health service; Telemedicine.
Pendahuluan: Telemedicine merupakan layanan kesehatan jarak jauh dengan memakai komunikasi audio, visual, dan data, termasuk perawatan, diagnosis, konsultasi, dan pengobatan, serta pertukaran data medis. Dalam pelaksanaan layanan telemedicine, diperlukan kerjasama dari berbagai pihak termasuk pasien dan fasilitas layanan kesehatan.
Tujuan: Menganalisis implementasi layanan telemedicine di masa pandemi Covid-19.
Metode: Penelitian literature review dengan database PubMed, ScienceDirect, dan Google Scholar. Penilaian dan kualitas artikel dalam penelitian ini menggunakan instrumen Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
Hasil: Berdasarkan hasil pencarian, didapatkan 9 artikel relevan dan sesuai dengan kriteria inklusi penelitian. Dari 9 artikel tersebut, diperoleh 5 hal terkait implementasi layanan telemedicine dan 3 faktor yang dapat memengaruhi layanan telemedicine.
Simpulan: 5 hal terkait implementasi layanan telemedicine yaitu kelebihan dan kekurangan, manfaat, faktor yang memengaruhi, dan implementasi layanan telemedicine pada masa pandemi Covid-19. Kemudian 3 faktor yang dapat memengaruhi layanan telemedicine yaitu keuangan, infrastruktur teknologi, serta aturan dan peraturan organisasi.
Keywords
References
Alvandi, M. (2017). Telemedicine and its role in revolutionizing healthcare delivery. The American Journal of Accountable Care. 5(1), e1-e5. Di akses dari: https://www.ajmc.com/view/telemedicine-and-its-role-in-revolutionizing-healthcare-delivery
Ashwood, S., Mehrotra, A., Cowling, D., & Uscher-Pines, L. (2017). Direct-to-consumer telehealth may increase access to care but does not decrease spending. Health Affairs (Project Hope), 36(3), 485–491. https://doi.org/10.1377/hlthaff.2016.1130
Baker, J. & Stanley, A. (2018). Telemedicine technology: A review of service, equipment, and other aspects. Current Alergy and Asthma Report. 18(11), 1-8. https://doi.org/10.1007/s11882-018-0814-6
Basit, S.A., Mathews, N., & Kunik, M.E. (2020). Telemedicine interventions for medication adherence in mental illness: A systematic review. General Hospital Psychiatry. 62, 28–36. https://doi.org/10.1016/j.genhosppsych.2019.11.004
Bendelin, N., Björkdahl, P., Risell, M., Nelson, K.Z., Gerdle, B., Andersson, G., & Buhrman, M. (2020). Patients’ experiences of internet-based acceptance and commitment therapy for chronic pain: A qualitative study. BMC Musculoskelet Disord. 21(1), 1–12. https://doi.org/10.1186/s12891-020-03198-1
Bull, T.P., Dewar, A.R., Malvey, D.M., & Szalma, J.L. (2016). Considerations for the telehealth systems of tomorrow: An analysis of student perceptions of telehealth technologies. JMIR Medical Education. 2(2), e11. https://doi.org/10.2196/mededu.5392
Chaet, D., Clearfield, R., Sabin, J.E., & Skimming, K. (2017). Ethical practice in telehealth and telemedicine. Journal of General Internal Medicine. 32(10), 1136–1140. https://doi.org/10.1007/s11606-017-4082-2
Chang, M.C. & Boudier-Reveret, M. (2020). Usefulness of telerehabilitation for stroke patients during the covid -19 pandemic. American journal of physical medicine & rehabilitation, 1-5. https://doi.org/10.1097/PHM.0000000000001468
Coelho, K.R. (2011). Identifying telemedicine service to improve access to specialty care for the underserved in the San Francisco safety net.International Journal of Telemedicine and Applications. Vol. 2011, 14 pages.https://doi.org/10.1155/2011/523161
Correi, A., Azevedo, V., & Lapao, L.V. (2017). Implementation of telemedicine in Cape Verde: Influencing factors. Acta Medica Portugues. 30(4), 255-62. https://doi.org/10.20344/amp.7578
Eccleston, C., Blyth, F.M., Dear, B.F., Fisher, E.A., Keefe, F.J., Lynch, M.E., Palermo, T.M., Reid, M.C., & Williams, A.C. (2020). Managing patients with chronic pain during the covid-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain. 161(5), 889–893. https://doi.org/10.1097/j.pain.0000000000001885
Ehrenreich, K., Kaller, S., Raifman, S., & Grossman, D. (2019). Women’s experiences using telemedicine to attend abortion information visits in Utah: A qualitative study. Women’s Heal Issues. 29(5), 407–413. https://doi.org/10.1016/j.whi.2019.04.009
Fortini, S., Espeche, A., & Caraballo, R. (2020). Telemedicine and epilepsy: A patient satisfaction survey of a pediatric remote care program. Epilepsy Research. 165, 106370. https://doi.org/10.1016/j.eplepsyres.2020.106370
Greenhalgh, T., Wherton, J., Shaw, S., & Morrison, C. (2020). Video consultations for covid-19. BMJ, 368, m998. https://doi.org/10.1136/bmj.m998
Hollander, J.E. & Carr, B.G. (2020). Virtually perfect? Telemedicine for covid-19. New England Journal of Medicine. 382(18), 1679-1681. https://doi.org/10.1056/NEJMp2003539
Kichloo, A., Albosta, M., Dettloff, K., Wani, F., El-Amir, Z., Singh, J., Aljadah, M., Chakinala, R.C., Kanugula, A.K., Solanki, S., & Chugh, S. (2020). Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Family Medicine and Community Health, 8(3), e000530. https://doi.org/10.1136/fmch-2020-000530
Kim, T. & Zuckerman, J.E. (2019). Realizing the potential of telemedicine in global health. Journal of Global Health, 9(2). https://doi.org/10.7189/jogh.09.020307
Kruse, C.S., Atkins, J.M., Baker, T.D., Gonzales, E.N., Paul, J.L., & Brooks, M. (2018). Factors influencing the adoption of telemedicine for treatment of military veterans with post-traumatic stress disorder. Journal of Rehabilitation Medicine. 50(5), 385-392. https://doi.org/10.2340/16501977-2302
Kumar, S., Kumar, A., Kumar, M., Kumar, A., Arora, R., & Sehrawat, R. (2020). Feasibility of telemedicine in maintaining follow-up of orthopaedic patients and their satisfaction: A preliminary study. Journal of Clinival Orthopaedics and Trauma. 11, S704–S710. https://doi.org/10.1016/j.jcot.2020.07.026
Lin, J.C., Crutchfield, J.M., Zurawski, D.K., & Stevens, C. (2018) Implementation of a virtual vascular clinic with point-of-care ultrasound in an integrated health care system. Journal of Vascular Surgery. 68(1), 213–218. https://doi.org/10.1016/j.jvs.2017.11.070
Mann, D.M., Chen, J., Chunara, R., Testa, P.A., & Nov, O. (2020). Covid-19 transforms health care through telemedicine: Evidence from the field. Journal of the American Medical Informatics Association. 27(7), 1132-1135. https://doi.org/10.1093/jamia/ocaa072
Mouchtouris, N., Lavergne, P., Montenegro, T.S., Gonzalez, G., Baldassari, M., Sharan, A., Jabbour, P., Harrop, J., Rosenwasser, R., & Evans, J.J. (2020). Telemedicine in neurosurgery: Lessons learned and transformation of care during the covid-19 pandemic. World Neurosurgery. 140, e387–e394. https://doi.org/10.1016/j.wneu.2020.05.251
Negrini, S., Kiekens, C., Bernetti, A., Capecci, M., Ceravolo, M.G., Lavezzi, S., Zampolini, M., & Boldrini, P. (2020). Telemedicine from research to practice during the pandemic. “Instant paper from the field” on rehabilitation answers to the Covid-19 emergency. Edizioni Minerva Medica. 56(3), 327-330. https://doi.org/10.23736/S1973-9087.20.06331-5
Nittari, G., Khuman, R., Baldoni, S., Pallotta, G., Battineni, G., Sirignano, A., Amenta, F., & Ricci, G. (2020). Telemedicine practice: Review of the current ethical and legal challenges. Telemedicine and e-Health. 26(12), 1427–1437. https://doi.org/10.1089/tmj.2019.0158
Ohannessian, R., Duong, T.A., & Odone, A. (2020). Global telemedicine implementation and integration within health systems to fight the covid-19 pandemic: A call to action. JMIR Public Health and Surveillance. 6(2), e18810. https://doi.org/10.2196/18810
Portnoy, J., Waller, M., & Elliott, T. (2020). Telemedicine in the era of covid-19. Journal of Allergy and Clinical Immunology Practice. 8(5), 1489-1491. https://doi.org/10.1016/j.jaip.2020.03.008
Satou, G.M., Rheuban, K., Alverson, D., Lewin, M., Mahnke, C., Marcin, J., Martin, G.R., Mazur, L.S., Shan, D.J., Shah, S., Tuckson, R., Webb, C.L., & Sable, C.A. (2017). Telemedicine in Pediatric cardiology: A scientific statement from the American Heart Association. The American Heart Association Journal, Circulation. 135(11), e648-e678. https://doi.org/10.1161/CIR.0000000000000478
Serper, M. & Volk, M.L. (2018). Current and future applications of telemedicine to optimize the delivery of care in chronic liver disease. Clinical Gastroenterology and Hepatology. 16(2), 157-161. https://doi.org/10.1016/j.cgh.2017.10.004
Smith, A.C., Thomas, E., Snoswell, C.L., Haydon, H., Mehrotra, A., Clemensen, J., & Caffery, L.J. (2020). Telehealth for global emergencies: Implications for corona virus disease 2019 (COVID-19). Journal of Telemedicine and Telecare, 26(5), 309-313. https://doi.org/10.1177/1357633X20916567
Song, X., Liu, X., & Wang, C. (2020). The role of telemedicine during the covid-19 epidemic in China-experience from Shandong province. Critical care, 24(1), 1-4. https://doi.org/10.1186/s13054-020-02884-9
Turolla, A., Rossettini, G., Viceconti, A., Palese, A., & Tommaso, G. (2020). Musculoskeletal physical therapy during the covid-19 pandemic: Is telerehabilitation the answer?. Physical Therapy & Rehabilitation Journal. 100(8), 1260-1264. https://doi.org/10.1093/ptj/pzaa093
Vidal-Alaball, J., Acosta-Roja, R., Hernandez, N.P., Luque, U.S., Morrison, D., Peres, N.S., Perez-Llano, J., Verges, A.S., & Segui F.L. (2020). Telemedicine in the face of the covid-19 pandemic. Atencion Primaria. 52(6), 418-422. https://doi.org/10.1016/j.aprim.2020.04.003
Williams, O.E., Elghenzai, S., Subbe, C., Wyatt, J.C., & Williams, J. (2017). The use of telemedicine to enhance secondary care: Some lessons from the front line. Future Healthcare Journal. 4(2), 109-14. https://doi.org/10.7861/futurehosp.4-2-109
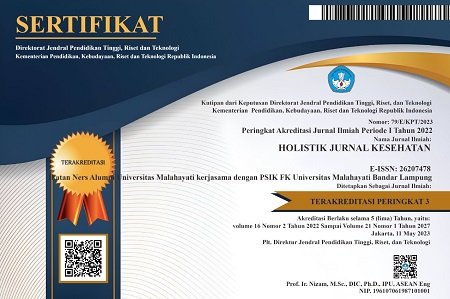
DOI: https://doi.org/10.33024/hjk.v16i3.7171
Refbacks
- There are currently no refbacks.
Copyright (c) 2022 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.