Analisis faktor-faktor yang berhubungan dengan kualitas hidup penderita hipertensi
Abstract
Background: The prevalence of hypertension in Lampung Province was 15.10 percent and the majority affects the pre-elderly and the elderly. The prevalence of hypertension in Pesisir Barat was 12.22 percent and at Puskesmas Krui was 21.19 percent. Treatment and care services for hypertension aim to improve the quality of life of patients. The purpose of this study was to analyze factors related to the quality of life of patients with hypertension in the posyandu for the elderly in the working area of the Puskesmas Krui Pesisir Barat.
Purpose: To determine the factors related to the quality of life of hypertensive patients in the Elderly Posyandu in the working area of the Krui Pesisir Barat Health Center.
Method: Quantitative with a cross-sectional design, a population of 998 people and a sample of 514 people with purposive sampling, then analyzed by chi square and logistic regression.
Results: Showed that there was a relationship between adherence to antihypertensive medication (p value <0.001 OR=2.0), physical activity (p-value <0.001 OR=5.5), comorbid disease (p-value <0.001 OR=4.2), stress level (p value <0.001 OR=2.6) with quality of life. The variable of physical activity became the variable with the most dominant influence on the quality of life with an OR of 4.4, followed by a comorbid variable with an OR of 2.9. Conclusion: physical activity is the most influential variable with the quality of life of hypertensive patients at the Elderly Posyandu with an OR of 4,4.
Suggestion: The management of the Pesisir Barat District Health Office to facilitate the elderly with hypertension in sports facilities such as green open spaces for the elderly for elderly gymnastics activities, conducting healthy walking competitions for the elderly and complete equipment such as sound systems for the continuity of the activities of the elderly posyandu, especially to improve the quality of life.
Conclusion: There is a relationship between the quality of life of patients with hypertension at the Posyandu for the elderly at the Krui Pesisisr Barat Public Health Center.
Keywords: Integrated Service for the Elderly; Hypertension; Quality of Life.
Pendahuluan: Prevalensi hipertensi di Provinsi Lampung 15,10 persen dan mayoritas diderita pra lansia dan lansia. Prevalensi hipertensi di Pesisir Barat sebesar 12,22 persen dan di Puskesmas Krui sebesar 21,19 persen. Pelayanan pengobatan dan perawatan hipertensi bertujuan meningkatkan kualitas hidup penderita. Tujuan dari penelitian ini adalah menganalisis factor yang berhubungan dengan kualitas hidup penderita hipertensi di posyandu lansia wilayah kerja Puskesmas Krui Pesisir Barat.
Tujuan: Untuk menganalisa faktor-faktor yang berhubungan dengan kualitas hidup penderita hipertensi di Posyandu Lansia Wilayah Kerja Puskesmas Krui Pesisir Barat.
Metode: Jenis penelitian kuantatif dengan rancangan potong lintang, populasi 998 orang dan sampel 514 orang dengan purposive sampling, lalu dianalisis dengan chi square dan regresi logistik.
Hasil: Hasil penelitian mendapatkan ada hubungan kepatuhan minum obat anti hipertensi (p value <0,001 OR=2,0), aktivitas fisik (p value <0,001 OR=5,5), adanya penyakit komorbid (p value <0,001 OR=4,2), tingkat stress (p value <0,001 OR=2,6) dengan kualitas hidup. Variabel aktivitas fisik menjadi variabel yang paling dominan pengaruhnya terhadap kualitas hidup dengan OR 4,4 disusul oleh variable komorbid dengan OR 2,9. Kesimpulan: aktivitas fisik merupakan variable yang paling berpengaruh dengan kualitas hidup penderita hipertensi di Posyandu Lansia dengan OR 4,4.
Saran: Dinas Kesehatan Kabupaten Pesisir Barat agar memfasilitasi lansia penderita hipertensi akan fasilitas olahraga seperti ruang terbuka hijau untuk lansia beraktivitas senam lansia, melakukan lomba jalan sehat bagi lansia serta peralatan kelengkapan alat seperti sound sistem untuk keberlangsungan kegiatan aktivitas posyandu lansia khususnya untuk meningkatkan kualitas hidup.
Simpulan: Terdapat hubungan Kualitas hidup penderita hipertensi di posyandu lansia Puskesmas Krui Pesisisr Barat.
Keywords
References
Alefishat, E., Jarab, A. S., & Farha, R. A. (2020). Factors affecting health-related quality of life among hypertensive patients using the EQ-5D tool.International Journal of Clinical Practice, 74(9), 0–3. https://doi.org/10.1111/ijcp.13532.
American Psychological Association. (2016). Revision of Ethical Standard 3.04 of the" Ethical Principles of Psychologists and Code of Conduct"(2002, as amended 2010). The American Psychologist, 71(9), 900.
Amir, M., Bar-On, D., & Penso, R. (1996). Positive—Negative Evaluation (PNE) scale: A new dimension of the subjective domains of quality of life measure. Quality of life Research, 5(1), 73-80.
Ayuningtyas, D. (2015). Kebijakan Kesehatan Prinsip dan Praktik (3rd ed.). Raja Grafindo Persada.
Az-Zahra, N. S., Yuswar, M. A., & Susanti, R. (2019).Perbedaan Kualitas Hidup Antara Pasien Hipertensi Dengan dan Tanpa Komplikasi di Puskesmas Alianyang Kota Pontianak Menggunakan European Quality of Life 5 Dimension (EQ-5D) Questionnaire.In Universitas Tanjung Pura. https://doi.org/10.2473/shigentosozai1953.83.947_421
Carvalho, J. L., Júnior, P. L. D., & Sant’Anna, A. S. (2017). Quality of working life and occupational stress: a Brazilian perspective. International Journal of Business Managemenent and Economic Research, 8(5), 1016-1025.
Chen, M. L., Hu, J., McCoy, T. P., Letvak, S., & Ivanov, L. (2018).Effect of a Lifestyle-Based Intervention on Health-Related Quality of Life in Older Adults with Hypertension. Journal of Aging Research, 2018, 1–9. https://doi.org/10.1155/2018/6059560
Cohen, S. (2020). Perceived Stress Scale (PSS). Encyclopedia of Behavioral Medicine, 1646–1648. https://doi.org/10.1007/978-3-030-39903-0_773
Dinas Kesehatan Kabupaten Pesisir Barat. (2020). Profil Kesehatan Kabupaten Pesisir Barat Tahun 2020.
EuroQol Research Foundation.(2020). EQ-5D-Y User Guide How to apply, score, and present results from the EQ-5D-Y Version. In euroqol.org (Version 2., Issue September). www.impact-test.co.uk.
Glover, C. M., Wang, Y., Fogelfeld, L., & Lynch, E. B. (2016). Stress and other determinants of diabetes-specific quality of life in low-income African Americans with uncontrolled type 2 diabetes mellitus. Journal of health care for the poor and underserved, 27(3), 1345-1356.
Gultom, A. B., Siregar, A. H., & Yahya, S. Z. (2018). Korelasi Stress dan Kualitas Hidup Pasien Hipertensi. Jurnal Kesehatan Vokasional, 3(2), 90. https://doi.org/10.22146/-.38151
Hastono, S. P. (2016). Analisis data pada bidang kesehatan.
Kementerian Dalam Negeri. (2011). Pedoman Pengintegrasian Layanan Sosial Dasar Di Pos Pelayanan Terpadu. Diakses dari: https://peraturan.bpk.go.id/Home/Details/111821/permendagri-no-19-tahun-2011.
Kementerian kesehatan Republik Indonesia (2021a). Petunjuk Teknis Pelaksanaan Posyandu Lanjut Usia dan Posbindu PTM Terintegrasi (1st ed.). Kemenkes RI. Diakses dari: https://www.scribd.com/document/512524075/juknis-posyandu-lansia-dan-posbindu-ptm-terintegrasi-ed-1-ori-file.
Kementerian Kesehatan Republik Indonesia .(2021b). Dampak Stres tidak hanya mengganggu kejiwaan namun juga berdampak pada kesehatan fisik. Http://P2ptm.Kemkes.Go.Id/. http://p2ptm.kemkes.go.id/infographic-p2ptm/stress/page/4/dampak-stres-tidak-hanya-mengganggu-kejiwaan-namun-juga-berdampak-pada-kesehatan-fisik
Kementerian kesehatan Republik Indonesia.(2013). Pedoman Teknis Penemuan dan Tatalaksana Hipertensi. In Direktorat Pengendalian Penyakit Tidak Menular Subdit Pengendalian Penyakit Jantung dan Pembuluh Darah. Kementerian Kesehatan Republik Indonesia. https://doi.org/10.1016/j.jash.2016.08.006.
Kementerian kesehatan Republik Indonesia.(2019). Hipertensi Penyakit Paling Banyak Diidap Masyarakat. Kemkes.Go.Id. https://www.kemkes.go.id/article/view/19051700002/hipertensi-penyakit-paling-banyak-diidap-masyarakat.html.
Kementerian kesehatan Republik Indonesia.(2019a). Laporan Provinsi Lampung RISKESDAS 2018. Lembaga Penerbit Badan Litbang Kesehatan.
Kementerian kesehatan Republik Indonesia.(2019b). Permenkes No 4 Tahun 2019 tentang Standar Teknis Pemenuhan Mutu Pelayanan Dasar Pada Standar Pelayanan Minimal Bidang Kesehatan.In Kemenkes Republik Indonesia.
Kementerian Kesehatan. (2020). Apa itu Hipertensi (Tekanan Darah Tinggi) ? P2ptm.Kemkes.Go.Id. http://p2ptm.kemkes.go.id/infographic/apa-itu-hipertensi-tekanan-darah-tinggi.
Kementerian kesehatan Republik Indonesia. (2018a). Aktivitas Fisik Berat. P2ptm.Kemkes.Go.Id. Direktorat Pencegahan dan Pengendalian Penyakit Tidak Menular, Direktorat Jenderal Pencegahan dan Pengendalian Penyakit, Kementrian kesehatan Republik Indonesia. Diakses dari: http://p2ptm.kemkes.go.id/infographic-p2ptm/obesitas/aktivitas-fisik-berat
Kementerian kesehatan Republik Indonesia. (2018b). Aktivitas Fisik Ringan. P2ptm.Kemkes.Go.Id. Direktorat Pencegahan dan Pengendalian Penyakit Tidak Menular, Direktorat Jenderal Pencegahan dan Pengendalian Penyakit, Kementrian kesehatan Republik Indonesia. Diakses dari: http://p2ptm.kemkes.go.id/infographic-p2ptm/obesitas/aktivitas-fisik-ringan
Kementerian kesehatan Republik Indonesia. (2018d). Manfaat aktivitas fisik. Manfaat Aktivitas Fisik. Direktorat Pencegahan dan Pengendalian Penyakit Tidak Menular, Direktorat Jenderal Pencegahan dan Pengendalian Penyakit, Kementrian kesehatan Republik Indonesia. Diakses dari: http://p2ptm.kemkes.go.id/infographic-p2ptm/hipertensi/manfaat-aktivitas-fisik
Khoirunnisa, S. M., & Akhmad, A. D. (2019).Quality of life of patients with hypertension in primary health care in Bandar Lampung. Indonesian Journal of Pharmacy, 30(4), 309–315. https://doi.org/10.14499/indonesianjpharm30iss4pp309
Kim, S. I. (2020). Factors Related to Hypertension Patients’ Quality of Life: The 7th Korean National Health and Nutrition Examination(1st Year, 2016). The Journal of Korean Society for School & Community Health Education, 21(1), 61–74. https://doi.org/10.35133/kssche.20200531.05.
Kurniawati, D. A., Adi, M. S., & Widyastuti, R. H. (2020). Tingkat Stres Lansia dengan Penyakit Tidak Menular. Jurnal Keperawatan Jiwa, 8(2), 123. https://doi.org/10.26714/jkj.8.2.2020.123-128
Liang, Z., Zhang, T., Lin, T., Liu, L., Wang, B., Fu, A. Z., Wang, X., Xu, X., Luo, N., & Jiang, J. (2019). Health-related quality of life among rural men and women with hypertension: assessment by the EQ-5D-5L in Jiangsu, China. Quality of Life Research, 28(8), 2069–2080. https://doi.org/10.1007/s11136-019-02139-3.
Lu, X., Juon, H.-S., He, X., Dallal, C. M., Wang, M. Q., & Lee, S. (2016). The association between perceived stress and hypertension among Asian Americans: does social support and social network make a difference? Physiology & Behavior, 176(1), 100–106. https://doi.org/10.1007/s10900-018-00612-7.
Manik, C. M., & Ronoatmodjo, S. (2019). Hubungan Diabetes Melitus dengan Hipertensi pada Populasi Obesitas di Indonesia (Analisis Data IFLS-5 Tahun 2014). Jurnal Epidemiologi Kesehatan Indonesia, 3(1), 19–24.
McKenzie, J. F., Neiger, B. L., & Thackeray, R. (2013). Planning, Implementing, & Evaluating Health Promotion Programs: A Primer (6th Edition) 6th Edition.
Morisky, D. E., Green, L. W., & Levine, D. M. (1986). Concurrent and Predictive Validity of Self Reported Measure of Medication Adherence. Med Care Vol. 24, 24(1), 67–74.
Peacock, E., Joyce, C., Craig, L. S., Lenane, Z., Holt, E. W., Muntner, P., & Krousel-Wood, M. (2021). Lowmedication adherence is associatedwith decline in health-related quality of life: Results of a longitudinal analysis among older women andmen with hypertension. Journal of Hypertension, 39(1), 153–161. https://doi.org/10.1097/HJH.0000000000002590.
Perrin, N. E., Davies, M. J., Robertson, N., Snoek, F. J., & Khunti, K. (2017). The prevalence of diabetes‐specific emotional distress in people with Type 2 diabetes: a systematic review and meta‐analysis. Diabetic Medicine, 34(11), 1508-1520.
Siregar, L. B., & Hidajat, L. L. (2017). Faktor yang berperan terhadap depresi, kecemasan dan stres pada penderita diabetes melitus tipe 2: studi kasus Puskesmas Kecamatan Gambir Jakarta Pusat. Manasa, 6(1), 15-22.
Valderas, J. M., Sibbald, B., & Salisbury, C. (2009).Defining Comorbidity: Implications for Understanding Health and Health Services. Annals of Family Medicine, 7(4), 357–363. https://doi.org/10.1370/afm.983.Martin
World Health Organization. (2012). WHOQOL User Manual.In World Health Organitation Quality Of Life (WHOQOL) (revvisi 1, Issue 1). https://doi.org/10.4091/iken1991.9.1_123.
World Health Organization. (2020). Physical activity.Who Newsroom. https://www.who.int/news-room/fact-sheets/detail/physical-activity
World Health Organization. (2021). Hypertension. Who.Int. https://www.who.int/news-room/fact-sheets/detail/hypertension.
World Health Organization. (2022). Ageing. Who.Int. https://www.who.int/health-topics/ageing#tab=tab_1.
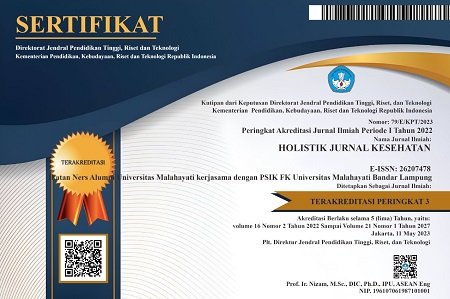
DOI: https://doi.org/10.33024/hjk.v16i7.8329
Refbacks
- There are currently no refbacks.
Copyright (c) 2022 Holistik Jurnal Kesehatan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.